The new anterior repair
Surgical Technique
Our vaginal surgical procedure was developed to 1) correctly identify the defect causing a cystocele and to identify the bladder protruding through the defect, and 2) repair the defect by reattaching the pubocervical fascia to its original supportive structures.
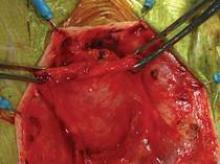
A full-thickness midline incision of the anterior vaginal epithelium is performed to enter the vesicovaginal space. The incision is carried up to the posterior urethral fold, and the vaginal epithelium is retracted laterally using a self-retaining ring retractor with hooks; this fully exposes the vesicovaginal space and the pubocervical fascia. The hooks attached to the retractor provide a level of traction and counter retraction for dissection and continual exposure of the surgical field that is hard to achieve with Allis clamps held by assistants. (We use a Lone Star ring retractor made by CooperSurgical, Trumbull, Conn.)
The pubocervical fascia is dissected and separated from the underside of the vaginal epithelium without splitting the vagina, as is done using traditional methods for midline plication. (See figure 8A.) The scissors are spread apart in the avascular lateral retroperitoneal space beneath the pubocervical fascia, and used to separate the fascia from the undersurface of the vagina to the pubic ramus. This is repeated on the other side of the dissection.
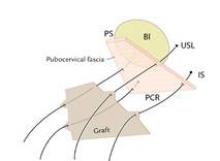
The surgeon can recognize the pubocervical fascia by its trapezoidal shape. Once the entire trapezoidal pubocervical fascia is identified, the presence of midline, paravaginal, or transverse defects can be identified and confirmed. (See figure 8B.)
In the absence of any midline or paravaginal defects with bladder protrusion or herniation, the possibility of a transverse defect can be evaluated by identifying the base of the pubocervical fascia. At this point, connective tissue adhesions are often seen between the pubocervical fascia and the prolapsed bladder and vagina. (See figure 9A.) We believe this is adhesive scar tissue that forms naturally after the trauma and mechanical damage of vaginal birth; its existence has not been truly recognized and/or well appreciated in the past.
When the adhesive scar is excised, the pubocervical fascia is freed up and can be easily separated from the bladder and vagina. (See figure 9B.) Allis clamps are placed on the lateral aspects of the pubocervical fascia and are lifted superiorly to expose the prolapsed bladder. (See figure 9C.) It is apparent at this point where the pubocervical fascia was originally attached to the pericervical ring. Correction of the bladder herniation can be demonstrated if the pubocervical fascia is elevated apically toward the pericervical ring (its previous attachment) and the retroperitoneal uterosacral ligaments. (See figure 9D.)
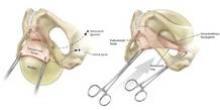
Permanent sutures of #0 Ethibond (Ethicon, Johnson & Johnson, Somerville, N.J.) are placed into each iliococcygeus fascia, or prespinous fascia, inferior to the ischial spine.
A suture of # 2-0 Ethibond is placed into each retroperitoneal uterosacral ligament as it attaches to the sacral periosteum at the level of S-2 or S-3 – a retroperitoneal uterosacral colpopexy. To do this, we use a pelvic reconstructive rectal pouch (American Medical Systems, Minnetonka, Minn.) that enables the index finger to be placed into the rectum for examination and palpation without contamination. The retroperitoneal uterosacral ligament is palpated at the level of the sacrum, where it attaches to the sacral periosteum, and a long Allis clamp is used to grasp the ligament. Each suture is placed from lateral to medial either through or around the ligament to avoid any entrapment of the ureter.
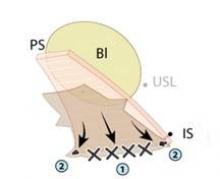
These sutures are held for placement into a piece of Surgisis Biodesign graft for anterior repair (Cook Medical, Bloomington, Ind.) that has been precut into a trapezoidal shape to fit the trapezoidal dissection of the pubocervical fascia.
The uterosacral sutures are placed into the superior nubbins on the lateral side of the graft and are held, and the prespinous (iliococcygeus) sutures of #0 Ethibond are placed through the graft’s lower nubbins and held. (See figure 11A.). We then place several sutures of #2-0 Ethibond into the base of the graft, then through the pubocervical fascia, and then the pericervical ring; tying these sutures repairs the transverse defect. (See figure 11B.) The lateral sutures are then tied, beginning with the prespinous sutures.