The new anterior repair
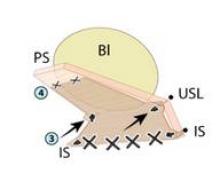
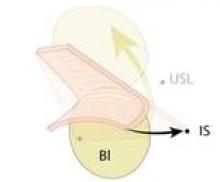
The graft is attached distally to the periurethral connective tissue with #2-0 Vicryl so that the graft lays flat against the pubocervical fascia. The bladder is now back in its normal anatomic position. (See figures 11C and 11D.)
Excess vaginal mucosa is then excised, and the vagina is closed in a running fashion with #2-0 Vicryl (Ethicon, Johnson & Johnson, Somerville, N.J.). An intraoperative cystoscopy is performed to document ureteral patency.
The Surgisis graft material is a biologic, recently Food and Drug Administration–approved graft that promotes tissue remodeling. I like using it because it safely provides more strength to the pubocervical fascia before it dissolves in 3-6 months, but the repair can be done alternatively without the graft – with sutures alone.
In our patient population of more than 500 patients followed for 24 months, we have had excellent results with 92% cure rate with sutures and 95% cure rates with Surgisis Biodesign. Some of these patients had previously failed midline plication and paravaginal repairs; the others had stage III or stage IV prolapse and had not undergone prior surgical repairs.
Surgeons who have been taught this new anterior repair have been excited and have found the technique easy to learn. However, only multicenter studies, currently in progress, and time will tell if this new technique will replace traditional anterior colporrhaphy.
Dr. Kovac is emeritus distinguished professor of gynecologic surgery at Emory University, Atlanta. He said he has no disclosures. To view a video of the surgery, visit SurgeryU at www.aagl.org/obgyn-news.