PART 1: Advising your patients Uterine fibroids: Childbearing, cancer, and hormone effects
Women who have uterine fibroids are often fearful about what the diagnosis means. Discussing the evidence with them provides reassurance for most.
IN THIS ARTICLE
CASE 1 RESOLVED What advice for Mrs. G.?
You order a gadolinium-enhanced, dynamic MRI scan and have blood drawn for total LDH and LDH isoenzymes. Total LDH and isoenzyme 3 are normal. MRI shows no increased enhancement of the fibroids on images taken 40 to 60 seconds after injection of gadolinium. You advise the patient that there is no evidence of cancer (sarcoma) and no urgent need for hysterectomy. You also tell her that, because she is symptomatic, myomectomy is an option that will preserve her uterus.
CASE 2 Fibroids, and contemplating childbearing
Mrs. H., a 35-year-old nulligravida, comes to the office for her first visit with you. She has no complaints, but your pelvic examination reveals a 10 week-size enlarged uterus. A sonogram shows a 6-cm subserosal fibroid and a 3-cm intramural fibroid near the endometrial cavity (see FIGURE). This patient was recently married and wants to become pregnant within the coming year.
When you tell Mrs. H. that she has fibroids, she grows concerned. She asks: “Will this affect my fertility, or a pregnancy?” and “Do I need surgery?”
You explain that the larger, subserosal fibroid is not a concern. The smaller, intramural fibroid could, however, have an impact on fertility and pregnancy if it distorts the uterine cavity.
To find out if that is the case, you order a saline infusion sonogram, which demonstrates, clearly, a normal cavity without distortion by the fibroid.
What is your advice to this woman?
Submucous fibroids that distort the uterine cavity decrease fertility; removal increases fertility. Otherwise, neither intramural nor subserosal fibroids appear to affect the fertility rate; removal has not been shown to increase fertility. Meta-analysis of 11 studies found that submucous myomas that distort the uterine cavity appear to decrease the pregnancy rate by 70% (relative risk [RR], 0.32; confidence interval [CI], 0.13–0.70).9
Assessing the uterine cavity. Evaluating a woman with fibroids for fertility requires reliable assessment of the uterine cavity. Hysteroscopy and saline infusion sonography have been shown to be far superior to transvaginal sonography or hysterosalpingography for detecting submucosal fibroids.10
The best modality for determining the extent of submucosal penetration of a myoma into the myometrium is MRI. It is also an excellent modality for evaluating the size, position, and number of multiple fibroids.11 The drawback to using MRI? It is more costly than other modalities.
Note: Classification of submucosal fibroids is based on the fraction of the mass within the cavity:
- Class 0 myomas are entirely intracavitary
- Class I myomas have 50% or more of the fibroid within the cavity
- Class II myomas have less than 50% within the cavity.12
Resection and fertility. Submucous fibroids can often be removed hysteroscopically. Systematic review of the evidence found that resection-restored fertility is equal to that of infertile controls undergoing in vitro fertilization who do not have fibroids (RR, 1.72; CI, 1.13–2.58).9 In that review, the presence of neither intramural nor subserosal fibroids decreased fertility (intramural: RR, 0.94, and CI, 0.73–1.20; subserosal: RR, 1.1, and CI, 0.06–1.72). Furthermore, removal of intramural and subserosal myomas by abdominal or laparoscopic myomectomy did not improve fertility. An updated unpublished meta-analysis, including studies published after 2001, came to the same conclusion (Pritts E, personal communication, 2008).
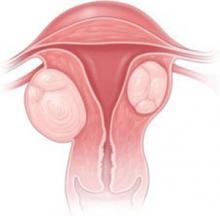
CASE 2: Subserosal, intramural myomas cause concern
In a woman contemplating childbearing, does a subserosal (left) or intramural (right) myoma present a problem because of potential to distort the uterine cavity?
Fibroids and pregnancy
The incidence of sonographically detected fibroids during pregnancy is low.13 Among 12,600 women at a prenatal clinic, routine second-trimester sonography identified myomas in 183 (mean age, 33 years)—an incidence of 1.5%.
Pregnancy has a variable and unpredictable effect on myoma growth, likely dependent on individual differences in genetics, circulating growth factors, and myoma-localized receptors. Most myomas do not, however, grow during pregnancy. A prospective study of pregnant women who had a single myoma found that 69% had no increase in volume throughout their pregnancy. In women who were noted to have an increase in the volume of their myoma, the greatest growth occurred before 10 weeks’ gestation. No relationship was found between initial myoma volume and myoma growth during the gestational period. 14
Do myomas complicate pregnancy?
Very rarely. Two studies reported on outcomes in large populations of pregnant women who were examined with routine second-trimester ultrasonography, with follow-up and delivery at the same institution.
In one of those studies, 12,600 pregnant women were evaluated, and the outcome in 167 women who were given a diagnosis of myoma was compared with the outcome in women who did not have a myoma.15 Despite similar clinical management between the two groups, no significant differences were seen in regard to the incidence of: