Sonography of ovarian masses: 9 key questions to guide clinical evaluation
Hallmark characteristics of benign and malignant lesions help point to the need for surgery. An expert sonologist details morphologic criteria that assist in diagnosis.
If the mass is within the ovary, a Brenner tumor, fibroma (FIGURE 1), granulosa cell tumor, or Sertoli-Leydig cell tumor should be considered. An ovarian fibroma may have significant attenuation9 and may contain calcifications.10 Solid masses are generally the smallest subset of ovarian tumors; approximately 10% are malignant.11
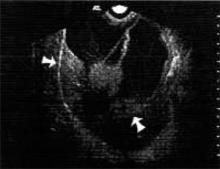
FIGURE 1 Fibroma
The well-demarcated hypoechoic mass in the right ovary is consistent with a fibroma.
Question 3 Is it a simple or complex cyst?
The risk that a simple, thin-walled cyst is malignant increases with patient age and the size of the cyst. Osmers et al11 found no malignancy in simple cysts removed from women 20 years of age or younger, while 3.6% of simple cysts were malignant in women over age 51.
As for size, Ekerhovd et al12 found no malignancies in simple cysts less than 2 cm in diameter, while 6.6% of simple cysts larger than 7.9 cm were found to be malignant. In general, simple ovarian cysts less than 5 cm in diameter are unlikely to be malignant.
While the risk of malignancy increases with complex ovarian cysts, these lesions are also more commonly benign. In an evaluation of 211 cystic-solid tumors, 29.4% were functional, 20.4% were retention cysts, 33.2% were benign neoplasms, and 17% were malignant.11 Color Doppler may improve diagnostic accuracy when a complex adnexal mass is detected.
Question 4Is the cyst loculated?
Although the risk of malignancy rises as loculated cysts become more complex, there is significant overlap between benign and malignant lesions.13 Mucinous cystadenomas (FIGURE 2) contain multiple septations and fluid with fine debris secondary to their thick mucinous content. A mucinous cystadenocarcinoma may contain papillary excrescences.14
FIGURE 2 Mucinous cystadenoma
Multiseptated, debris-filled mucinous cystadenoma in the left ovary of a 20-year-old patient.
Question 5 Are papillary excrescences present?
These represent localized overgrowth of the epithelium. The likelihood of malignancy rises as the number of excrescences increases (FIGURE 3).15 Papillary projections into the cyst cavity of less than 3 mm are not strongly associated with malignancy.16
Because of the proportionally larger surface area that must be examined, the likelihood of missing a papillary excrescence increases with the size of the cyst.12 Ranney and Ahmad17 have reported significantly reduced survival when an ovarian neoplasm contains papillary excrescences.
FIGURE 3 Papillary excrescences
Multiseptated 14-cm endometrioid adenocarcinoma containing several papillary excrescences (arrows).
Question 6Are there echo-dense foci?
Because fat mixed with hair produces echogenic foci with acoustic shadowing, the echo-dense foci in benign cystic teratomas are usually easily identifiable (FIGURE 4). In fact, morphologic assessment alone has a sensitivity of 93.1% for the detection of benign cystic teratomas.18 Be aware, however, that some malignant tumors may have components that cast an acoustic shadow.19
Benign cystic teratomas grow at a mean rate of 1.8 mm per year in premenopausal women,20 and 72% of cystic teratomas are avascular.18 If the solid components of an apparent benign cystic teratoma have vascular flow, a struma ovarii consisting largely of thyroid tissue should be considered.21
FIGURE 4 Benign cystic teratoma
Complex cystic/solid benign cystic teratoma. Note that part of the ovary is unaffected.
Question 7Is there echogenicity of interior fluid?
If so, it may provide a clue to diagnosis. For example, a serous cyst generally contains clear fluid, while mucinous cysts contain fine debris. An endometrioma tends to contain homogeneous debris22(FIGURE 5), while a hemorrhagic cyst may have a ground-glass appearance (FIGURE 6). Echogenic particles within a hypoechoic background are characteristic of a benign cystic teratoma.
FIGURE 5 Homogeneous debris
The homogeneous debris in this left ovarian mass is consistent with an endometrioma.
FIGURE 6 Hemorrhagic cyst
Ground-glass appearance of a hemorrhagic ovarian cyst.
Question 8Is measurable fluid in the cul-de-sac?
As the ovaries become atrophic, the production of cul-de-sac fluid declines. A post-menopausal patient has 5.5±7.8 mL of cul-de-sac fluid, depending on the degree of ovarian activity.23 Since transvaginal ultrasound can consistently detect 8 mL or more of cul-de-sac fluid, no fluid is identified in the majority of postmenopausal patients.24 Thus, a moderate amount of cul-de-sac fluid in a postmenopausal patient should raise the sonologist’s index of suspicion concerning a possible ovarian tumor.
Question 9How does the mass change over time?
The architectural pattern of ovarian masses is frequently dynamic. For example, between 53% and 89% of functional cysts spontaneously regress.11 Thus, a follow-up ultrasound examination in 6 to 8 weeks may provide additional information about a mass’s etiology. Repeat sonography is recommended in cases without obvious stigmata of malignancy or a size that would mandate surgery.