Translating AHA/ACC cholesterol guidelines into meaningful risk reduction
The new recommendations detail refined, personalized lipid management and emphasize multiple levels of evidence. The result? Care is more complex but patients might benefit more.
PRACTICE RECOMMENDATIONS
› Reduce the low-density lipoprotein cholesterol (LDL-C) level in patients with clinical atherosclerotic cardiovascular disease (ASCVD) using high-intensity statin therapy or maximally tolerated statin therapy. A
› Use an LDL-C threshold of 70 mg/dL to prompt consideration of adding nonstatin therapy in patients who have very high-risk ASCVD. A
› Start high-intensity statin therapy in patients who have primary hypercholesterolemia (LDL-C level ≥ 190 mg/dL) without calculating the 10-year ASCVD risk. A
› Begin moderate-intensity statin therapy in patients 40 to 75 years of age who have diabetes mellitus and an LDL-C level ≥ 70 mg/dL without calculating 10-year ASCVD risk. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
In patients > 75 years of age with clinical ASCVD, it is reasonable to initiate or continue moderate- or high-intensity statin therapy after evaluation of the potential for ASCVD risk reduction, adverse effects, and drug–drug interactions, as well as patient frailty and patient preference.1
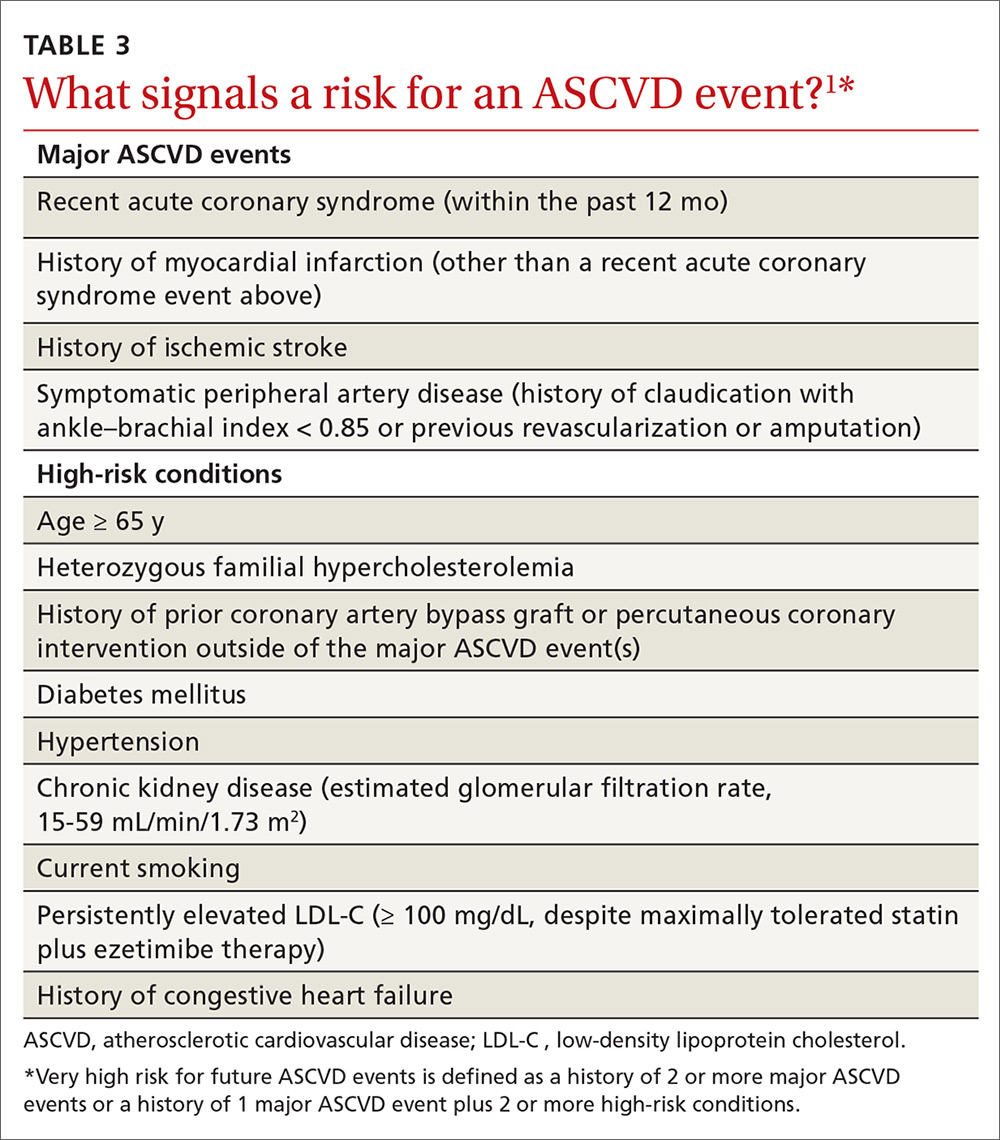
Very high risk. In patients at very high risk (this includes a history of multiple major ASCVD events or 1 major ASCVD event plus multiple high-risk conditions), maximally tolerated LDL-C-lowering therapy should include maximally tolerated statin therapy and ezetimibe before considering a PCSK9 inhibitor. An LDL-C level ≥ 70 mg/dL or a non-HDL-C level ≥ 100 mg/dL is considered a reasonable threshold for adding a PCSK9 inhibitor to background lipid-lowering therapy1 (TABLE 31).
Heart failure. In patients with heart failure who have (1) a reduced ejection fraction attributable to ischemic heart disease, (2) a reasonable life expectancy (3-5 years), and (3) are not already on a statin because of ASCVD, consider initiating moderate-intensity statin therapy to reduce the risk for an ASCVD event.1
Reduction of elevated triglycerides
The guideline defines moderate hypertriglyceridemia as a nonfasting or fasting TG level of 175 to 499 mg/dL. Such a finding is considered a risk-enhancing factor and is 1 of 5 components of the metabolic syndrome. Three independent measurements are advised to diagnose primary moderate hypertriglyceridemia. Severe hypertriglyceridemia is diagnosed when the fasting TG level is ≥ 500 mg/dL.1
In moderate hypertriglyceridemia, most TGs are carried in very-low-density lipoprotein particles; in severe hypertriglyceridemia, on the other hand, chylomicrons predominate, raising the risk for pancreatitis. In adults with severe hypertriglyceridemia, therefore—especially when the fasting TG level is ≥ 1000 mg/dL—it is reasonable to identify and address other causes of hypertriglyceridemia. If TGs are persistently elevated or increasing, levels should be reduced to prevent acute pancreatitis with a very low-fat diet and by avoiding refined carbohydrates and alcohol; consuming omega-3 fatty acids; and, if necessary, taking a fibrate.1
Continue to: In adults...