Data Trends 2025: Mental Health





Reviewed by: Jason C. DeViva, PhD, Associate Professor, Department of Psychiatry,
Yale School of Medicine, New Haven, Connecticut; Clinical
Psychologist; Co-Director, PTSD Clinical Team, VA Connecticut
Health Care System, West Haven, Connecticut
Dr. DeViva has disclosed no relevant financial relationships.





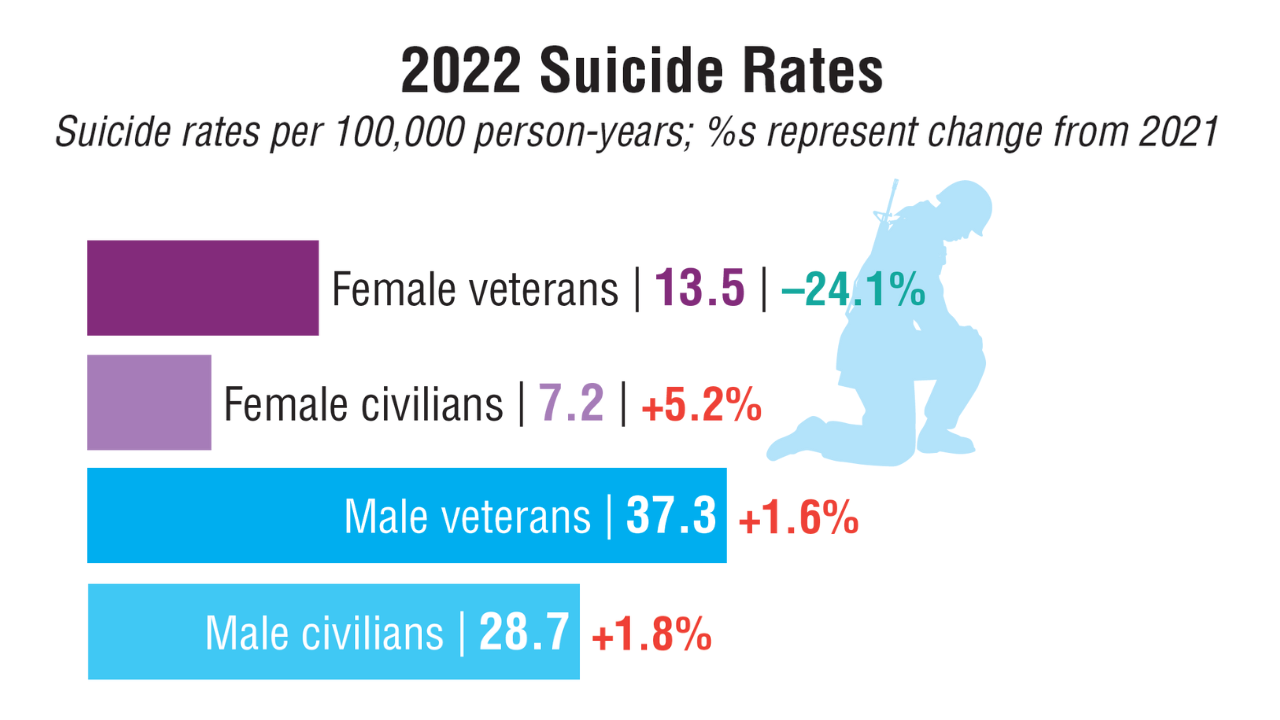
Suicide is the second leading cause of death for US veterans aged 18 to 44 years.1 The 2024 National Veteran Suicide Prevention Annual Report disclosed that of the 6407 veterans who died from suicide in 2022, 60% had a prior mental health diagnosis.1 The report showed improved suicide rates among veterans with certain mental health conditions, such as depression, PTSD, and anxiety, from 2001 to 2022, potentially due to expanded mental health care access for patients with trauma and increased telehealth availability.1,2 For conditions like PTSD, receiving first-line evidence-based treatment also lowered suicide risk.3 Veteran suicide rates have risen 16.2% for those with opioid use disorder since 2001, while falling 13.7% for alcohol use disorder—though the latter rose 1.2% between 2021 and 2022.1
If you or someone you know is having thoughts of suicide, call or text 988 to reach out to the National Suicide Prevention Lifeline, or contact the Veterans Crisis Line: www.veterancrisisline.net.
 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1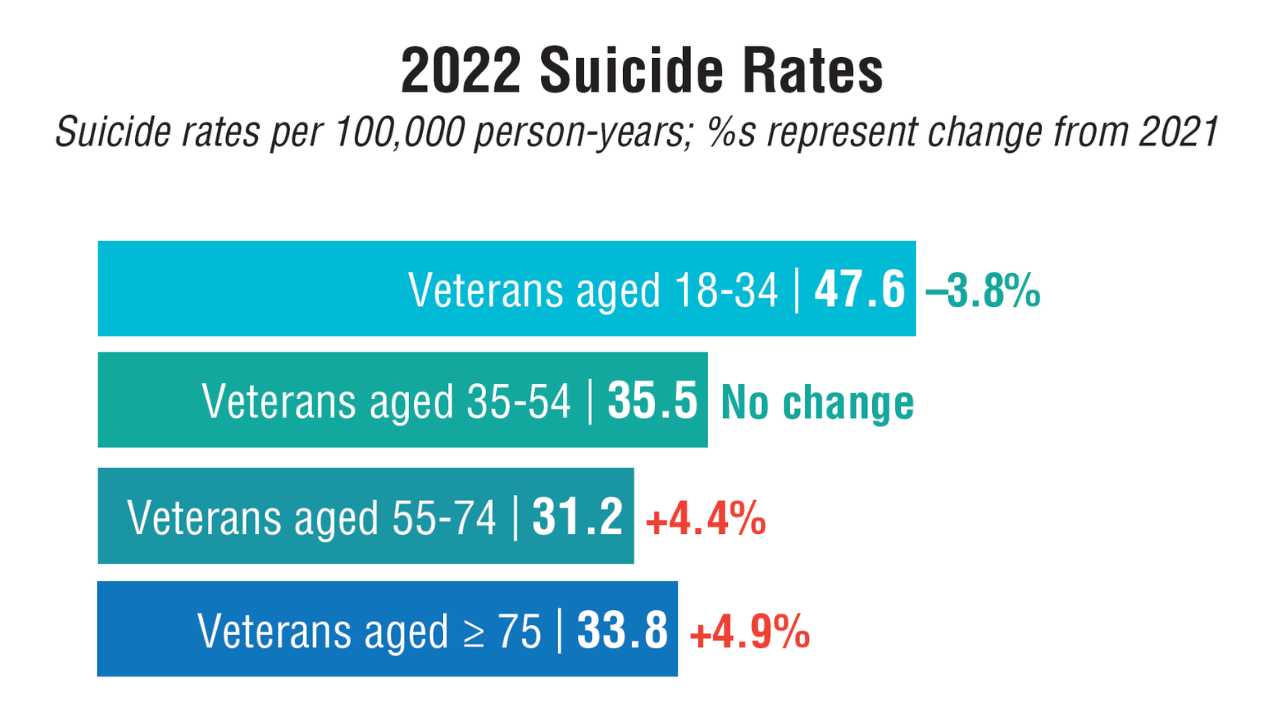 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1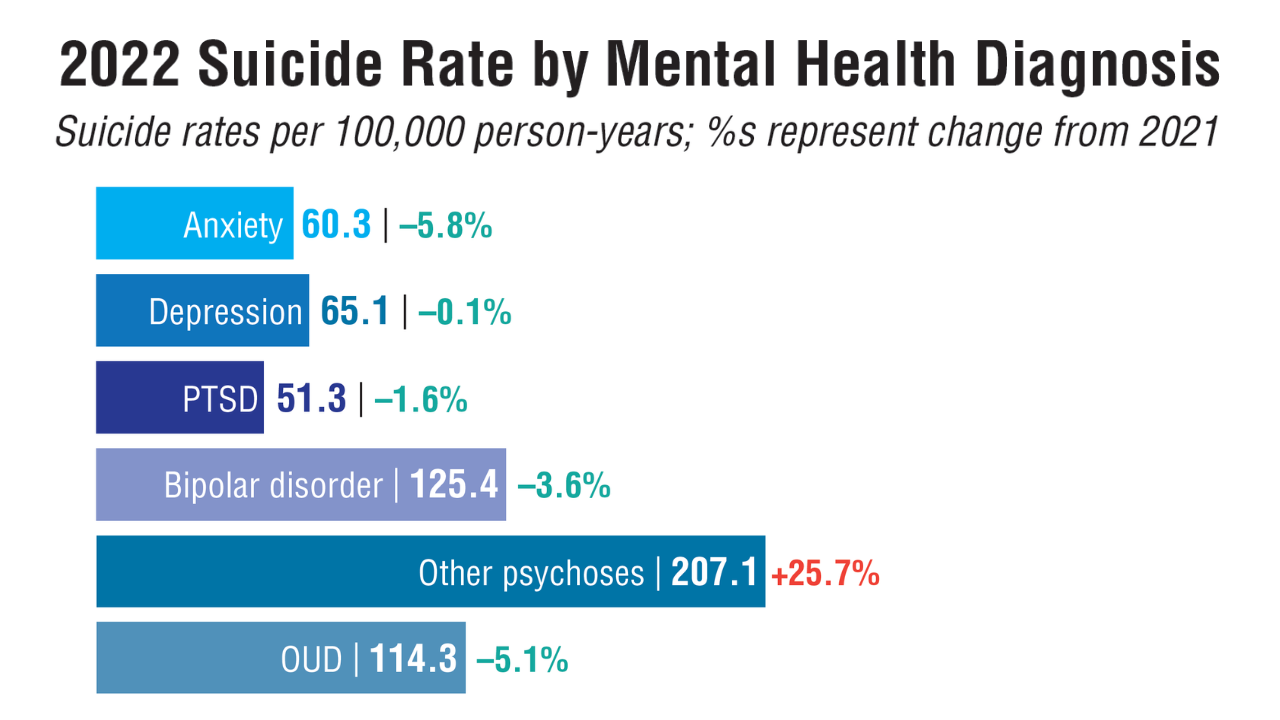 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1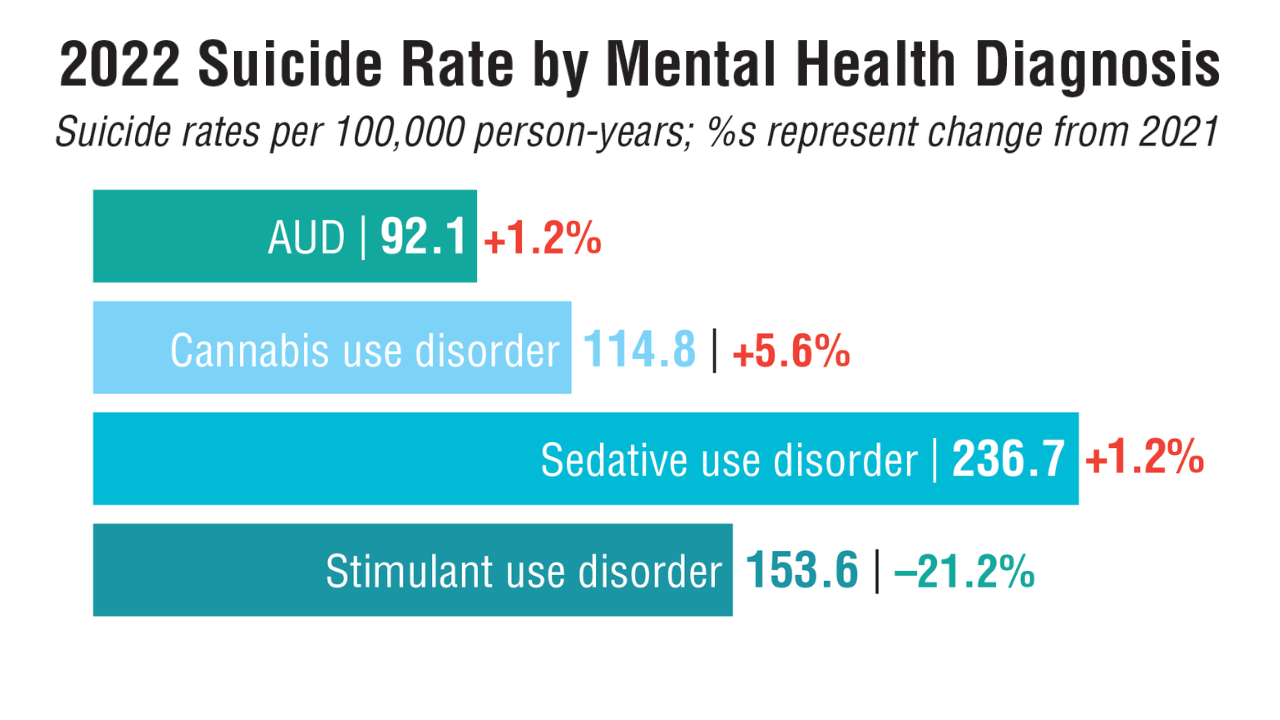 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1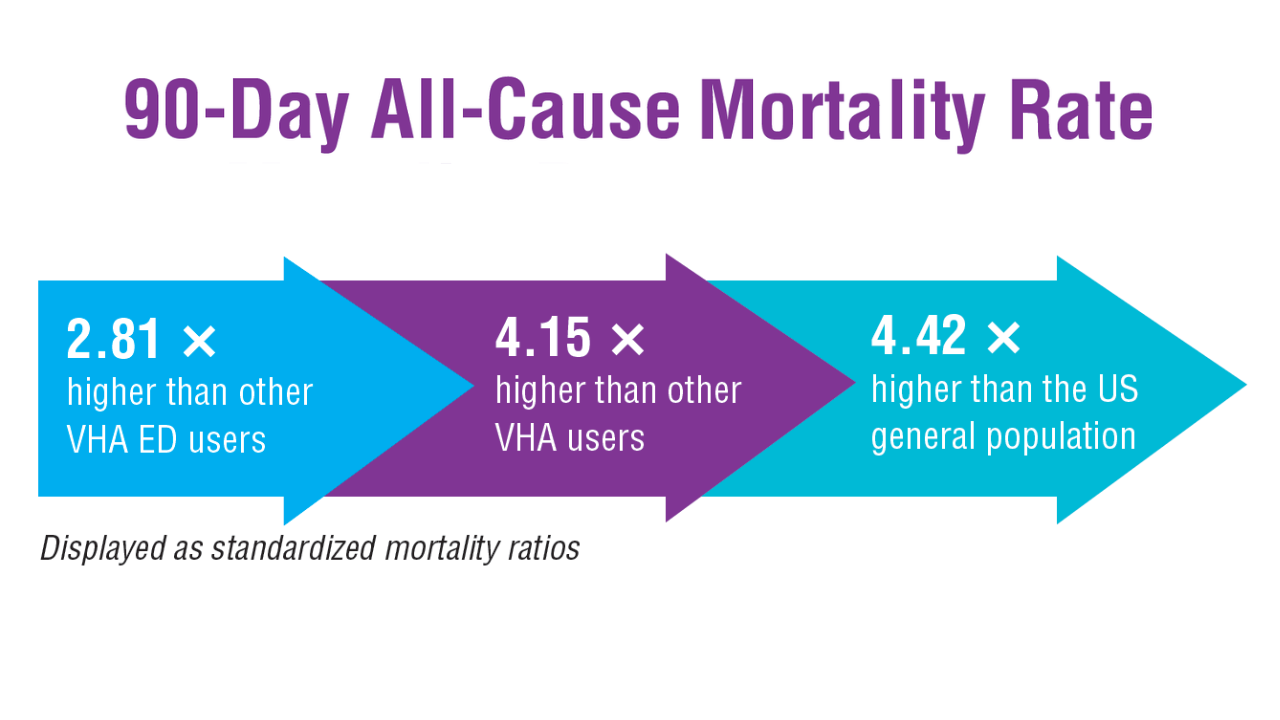 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4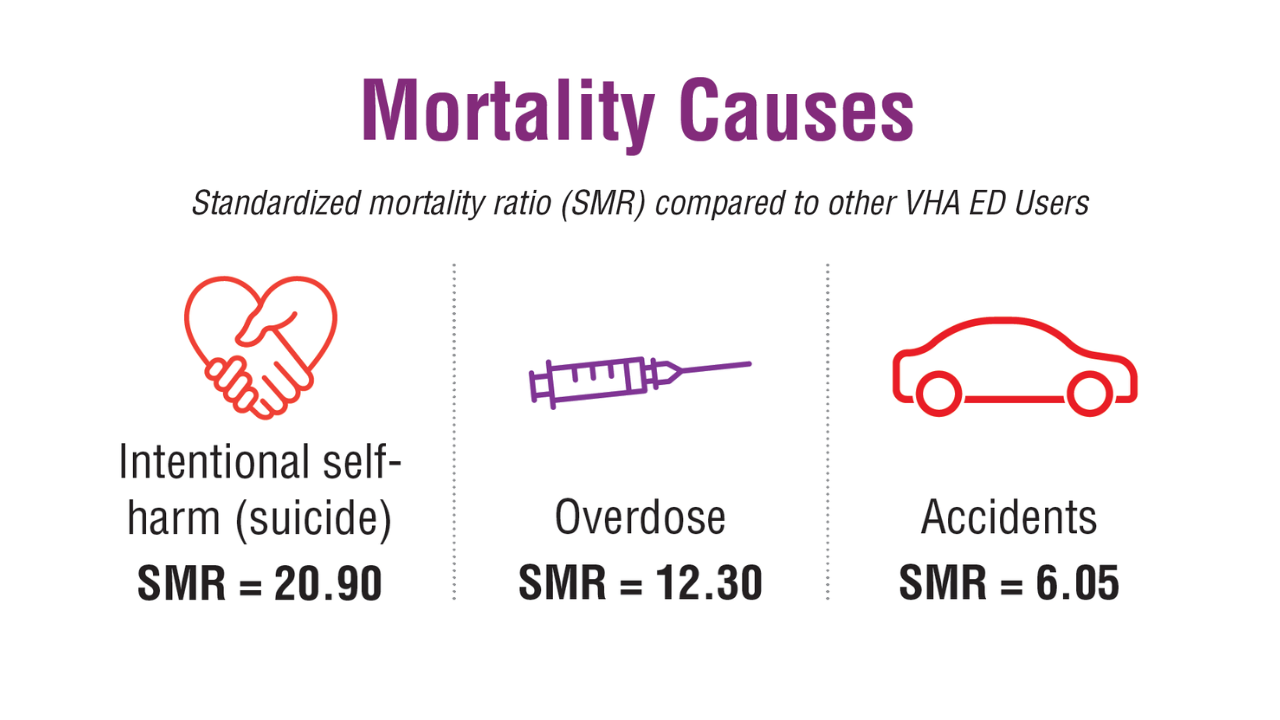 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4
In a cohort of nearly 180,000 veterans with more than 300,000 high-risk emergency department (ED) visits for suicidality or overdose, more than 2% died within 90 days of their hospitalization.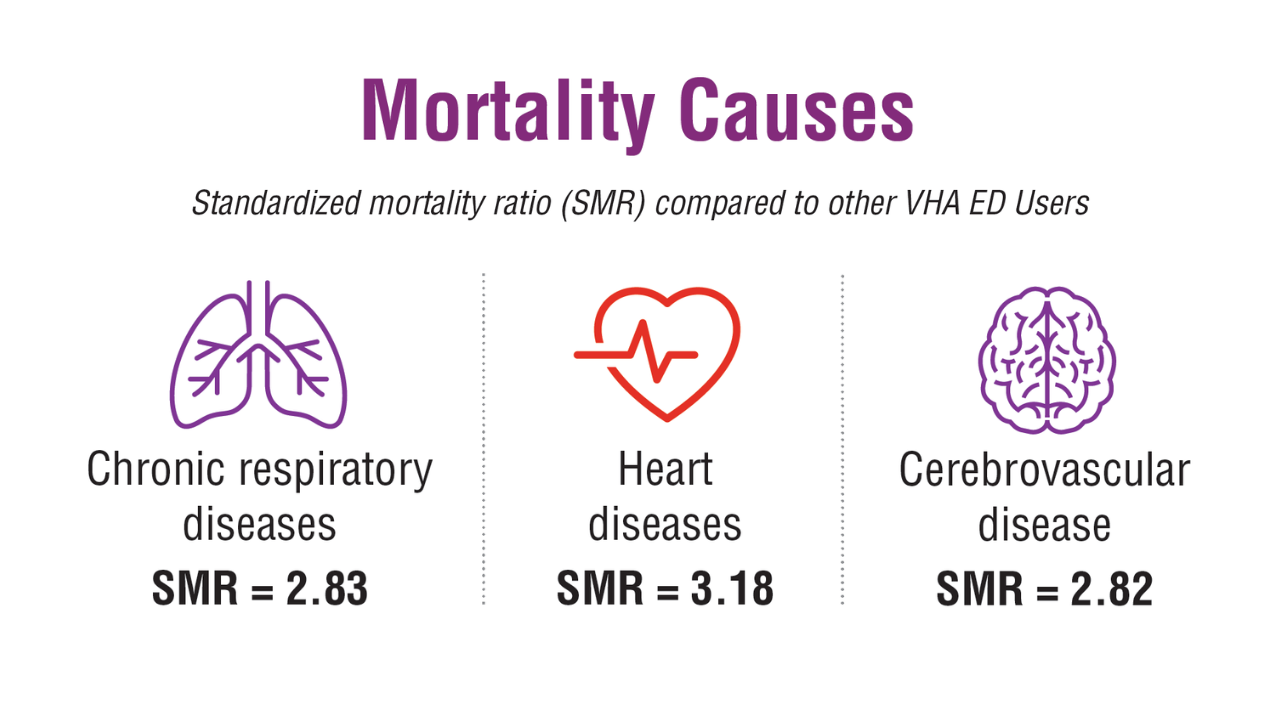 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4
Patients with high-risk ED visits had increased mortality rates compared to other VHA ED users, other VHA users, and the US general population. This increase was highest in Asian or Pacific Islander and White veterans (SMR = 3.50, SMR = 3.11, respectively, compared to other VHA ED users).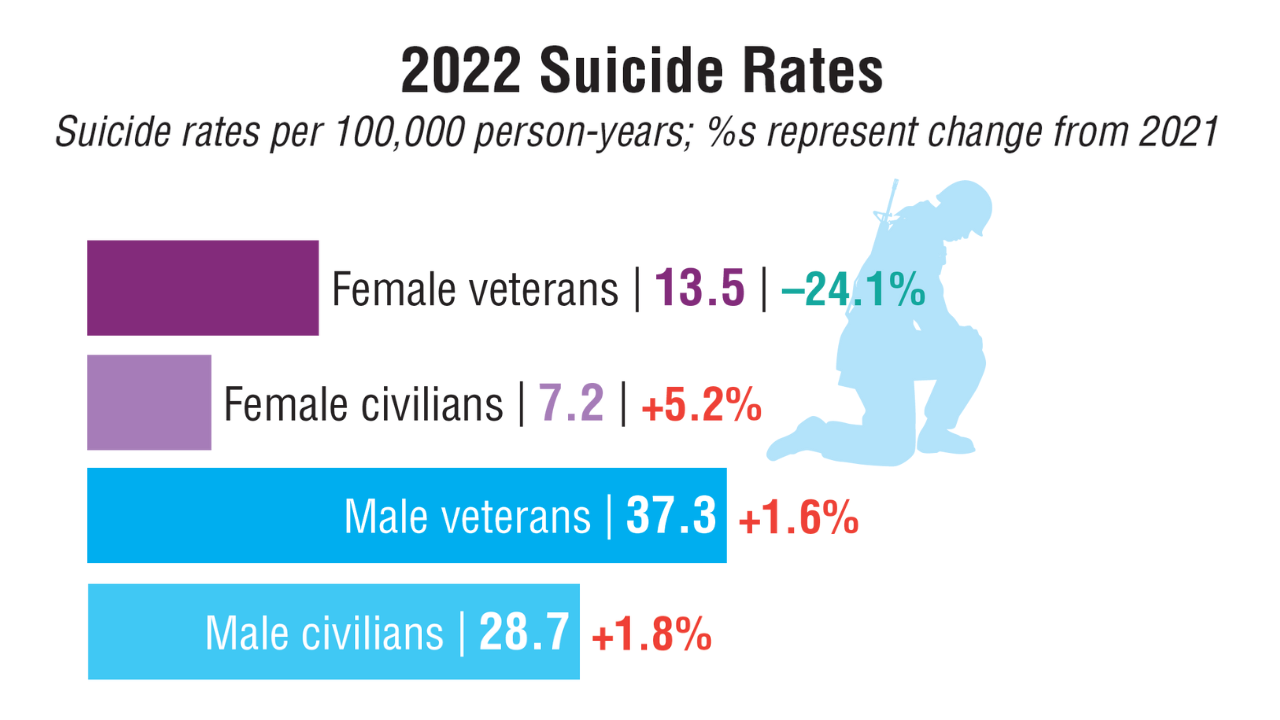 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1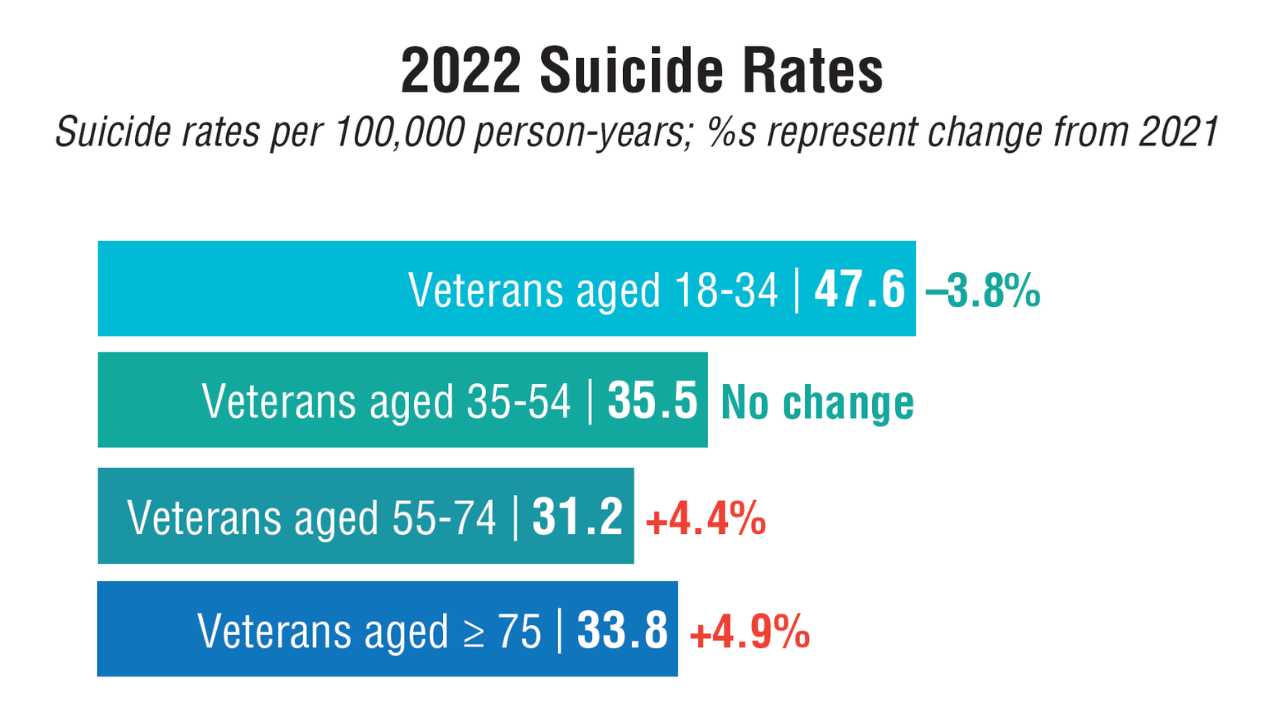 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1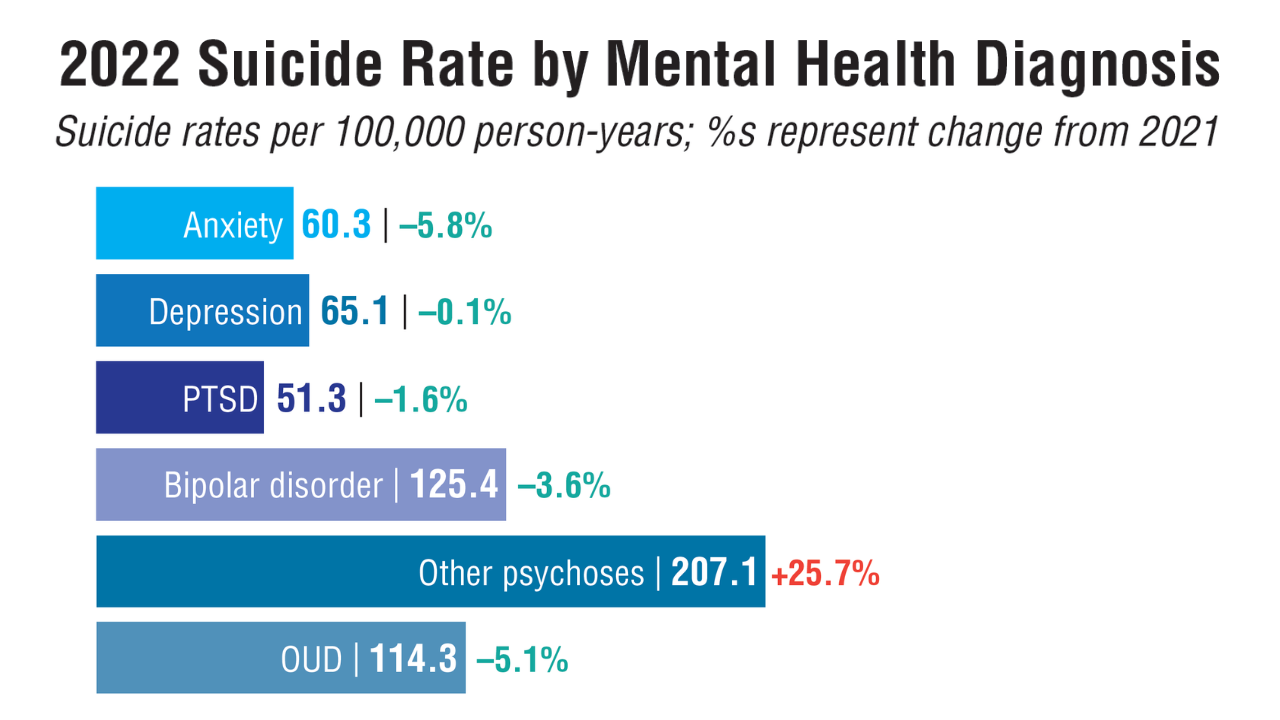 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1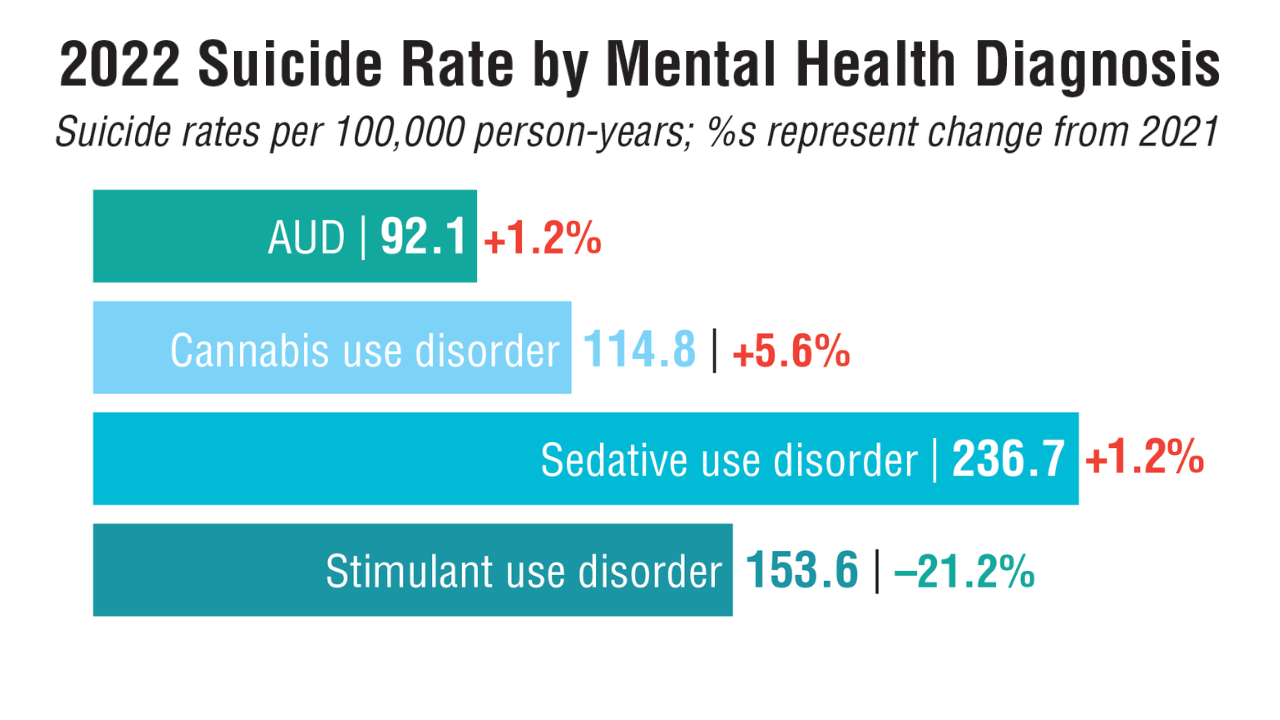 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1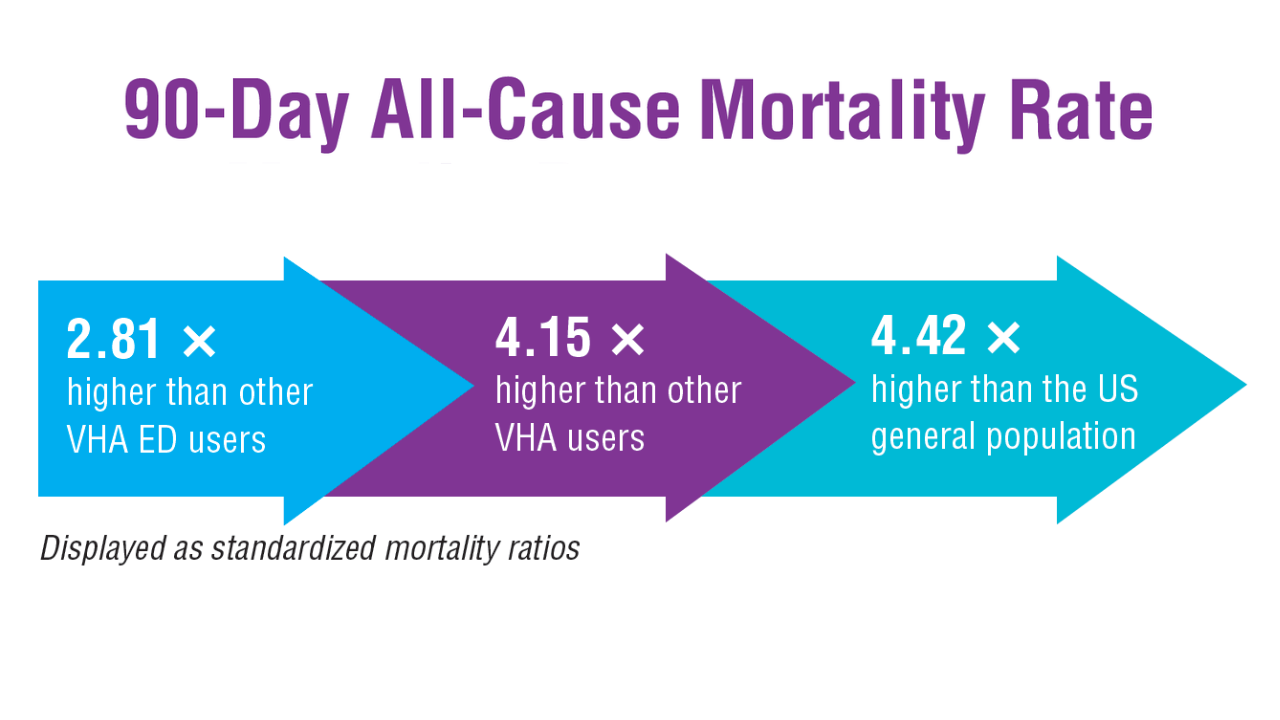 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4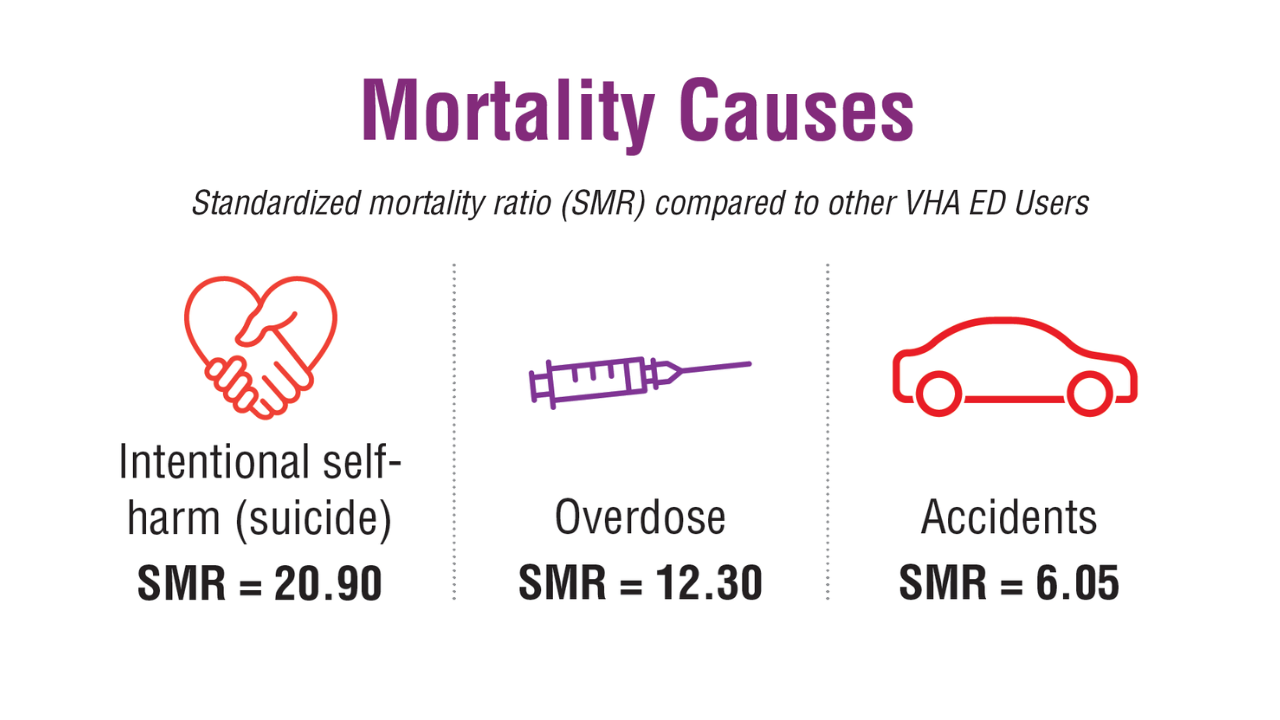 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4
In a cohort of nearly 180,000 veterans with more than 300,000 high-risk emergency department (ED) visits for suicidality or overdose, more than 2% died within 90 days of their hospitalization.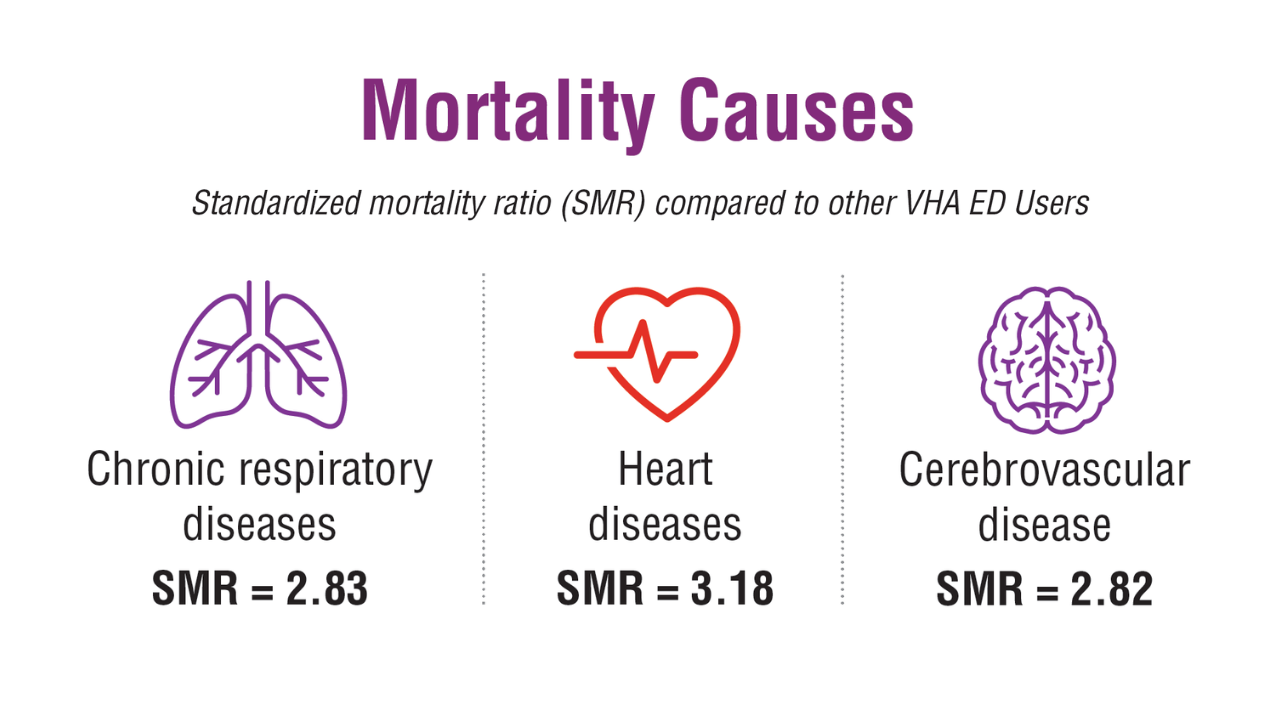 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4
Patients with high-risk ED visits had increased mortality rates compared to other VHA ED users, other VHA users, and the US general population. This increase was highest in Asian or Pacific Islander and White veterans (SMR = 3.50, SMR = 3.11, respectively, compared to other VHA ED users).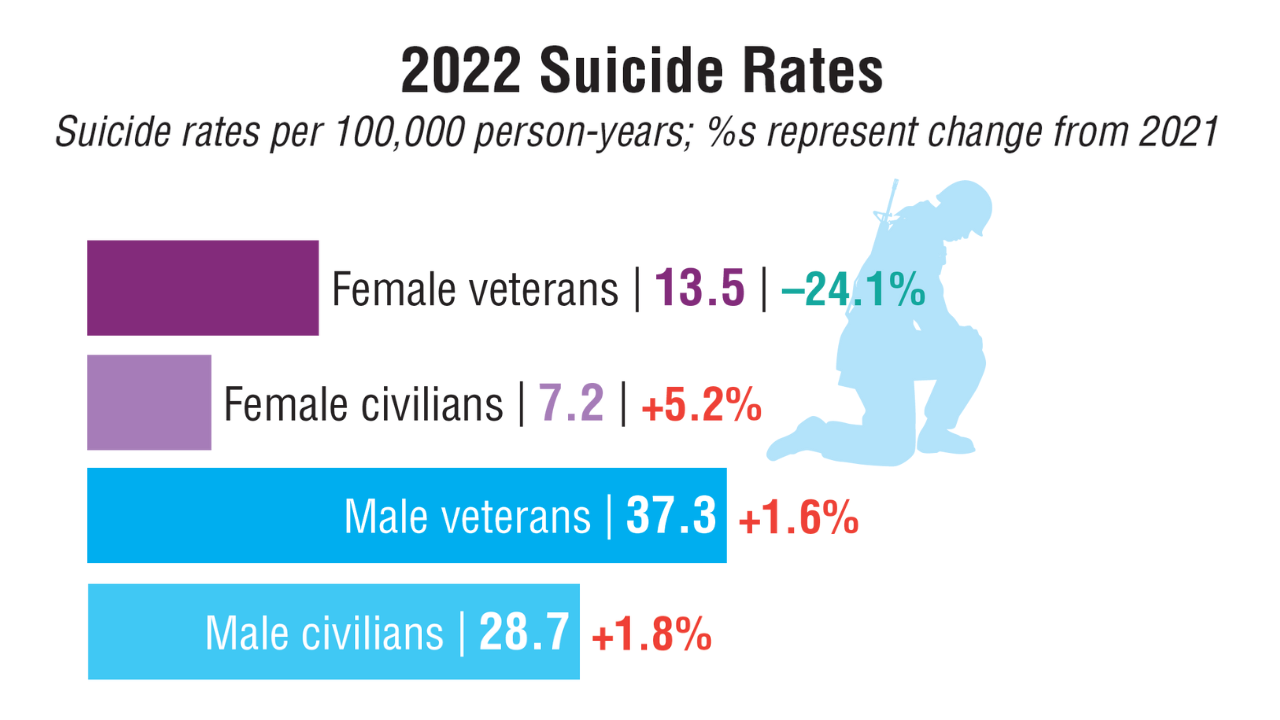 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1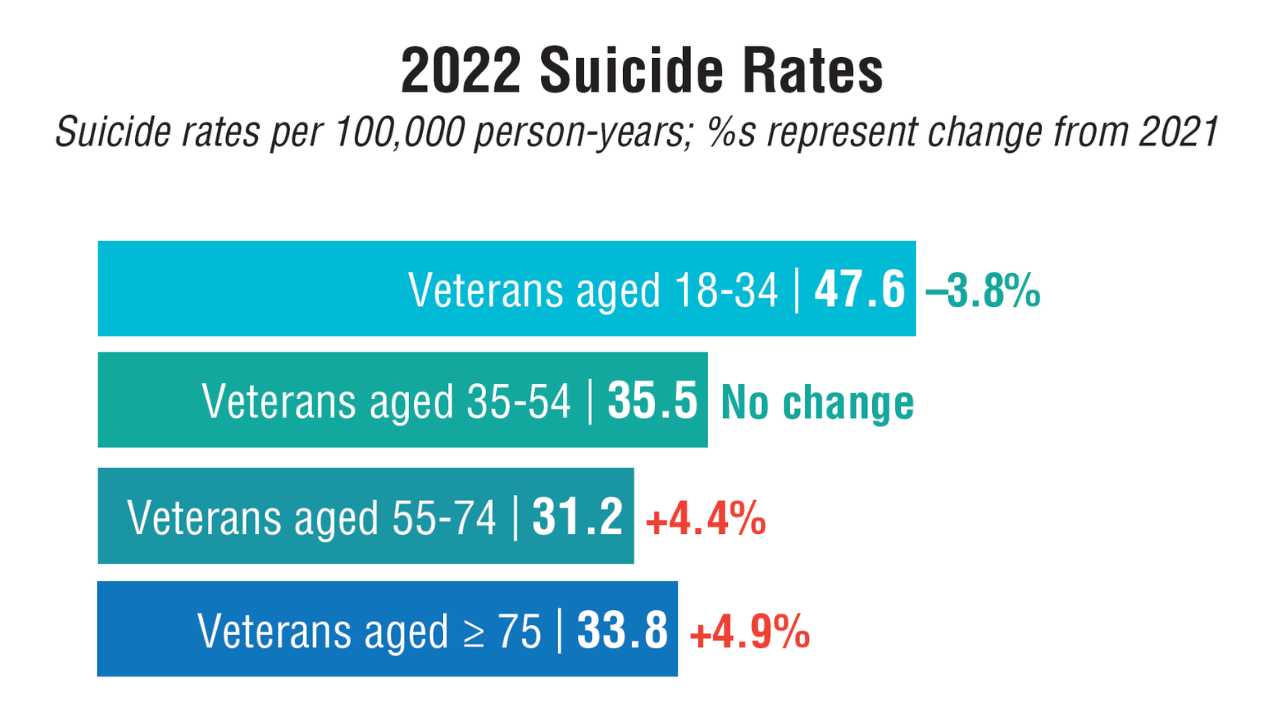 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1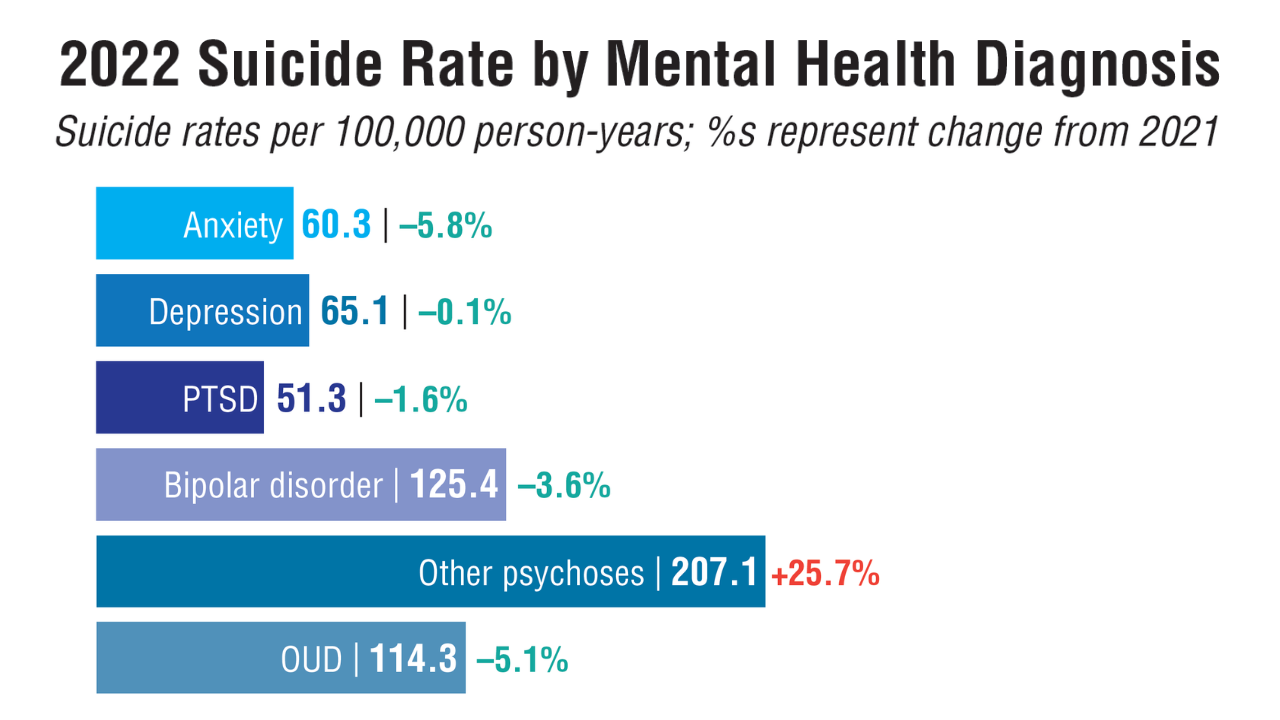 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1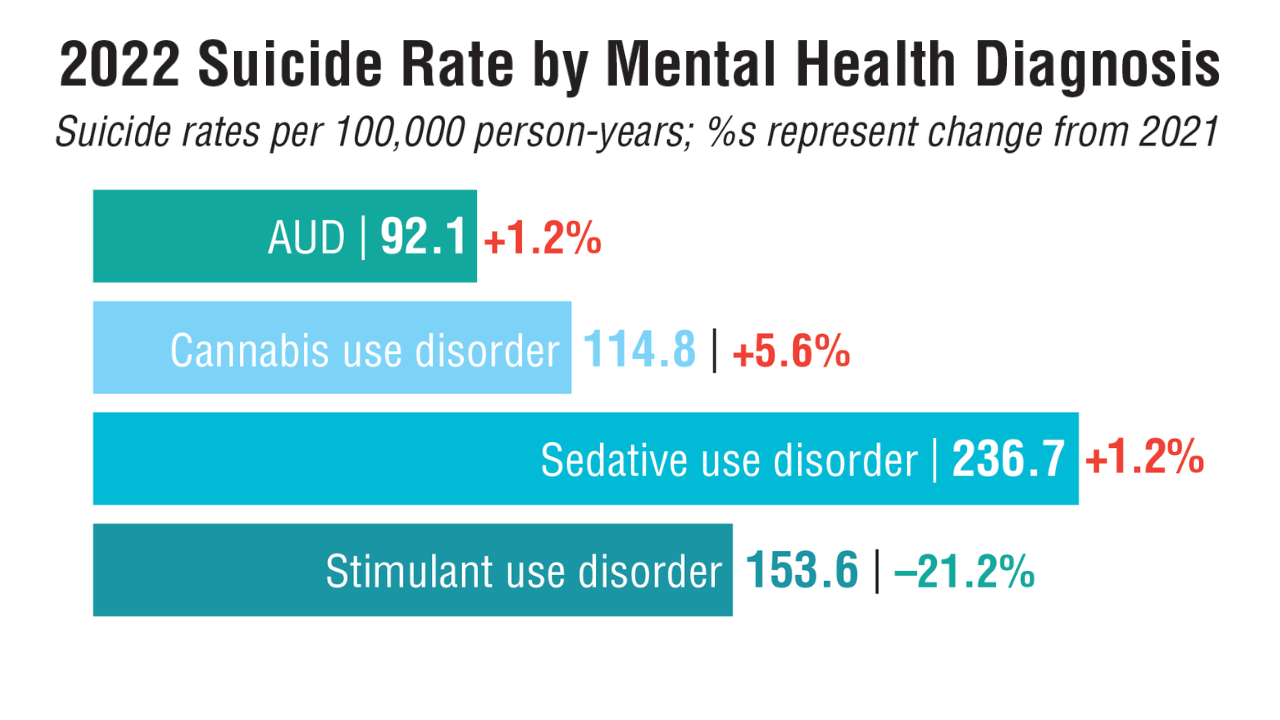 Veteran Suicide and Mental Health Trends1
Veteran Suicide and Mental Health Trends1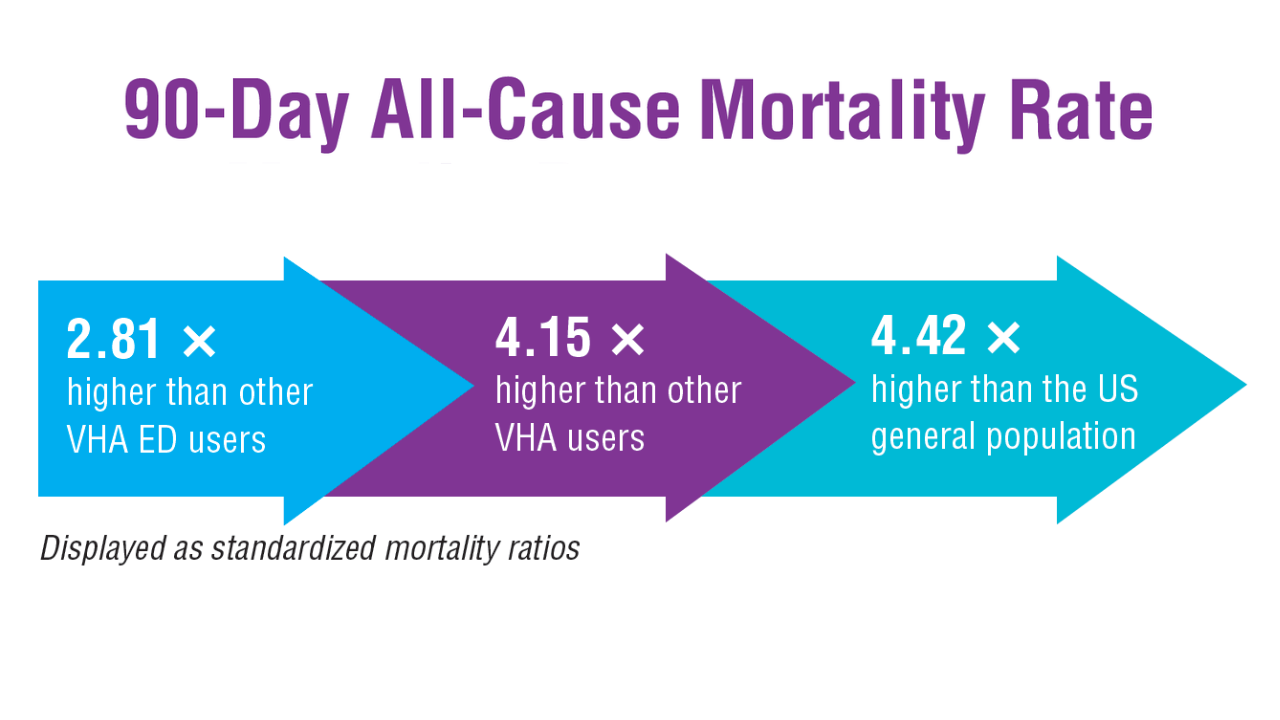 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4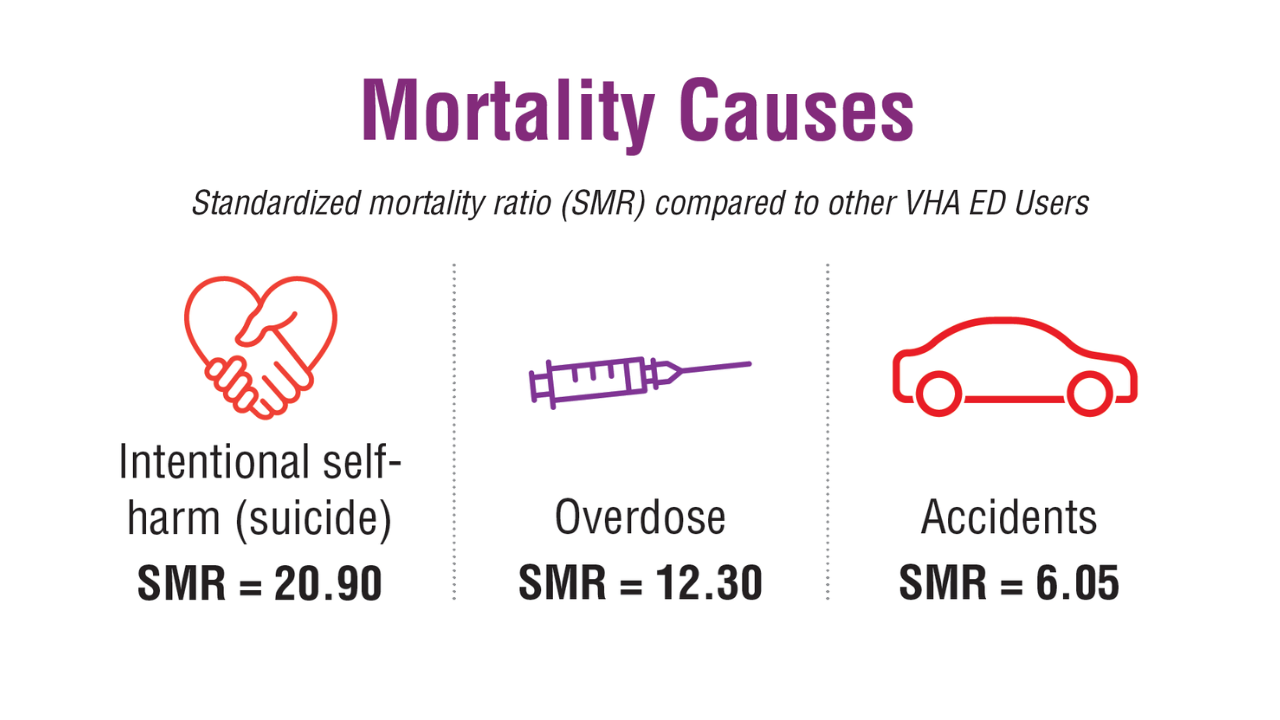 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4
In a cohort of nearly 180,000 veterans with more than 300,000 high-risk emergency department (ED) visits for suicidality or overdose, more than 2% died within 90 days of their hospitalization.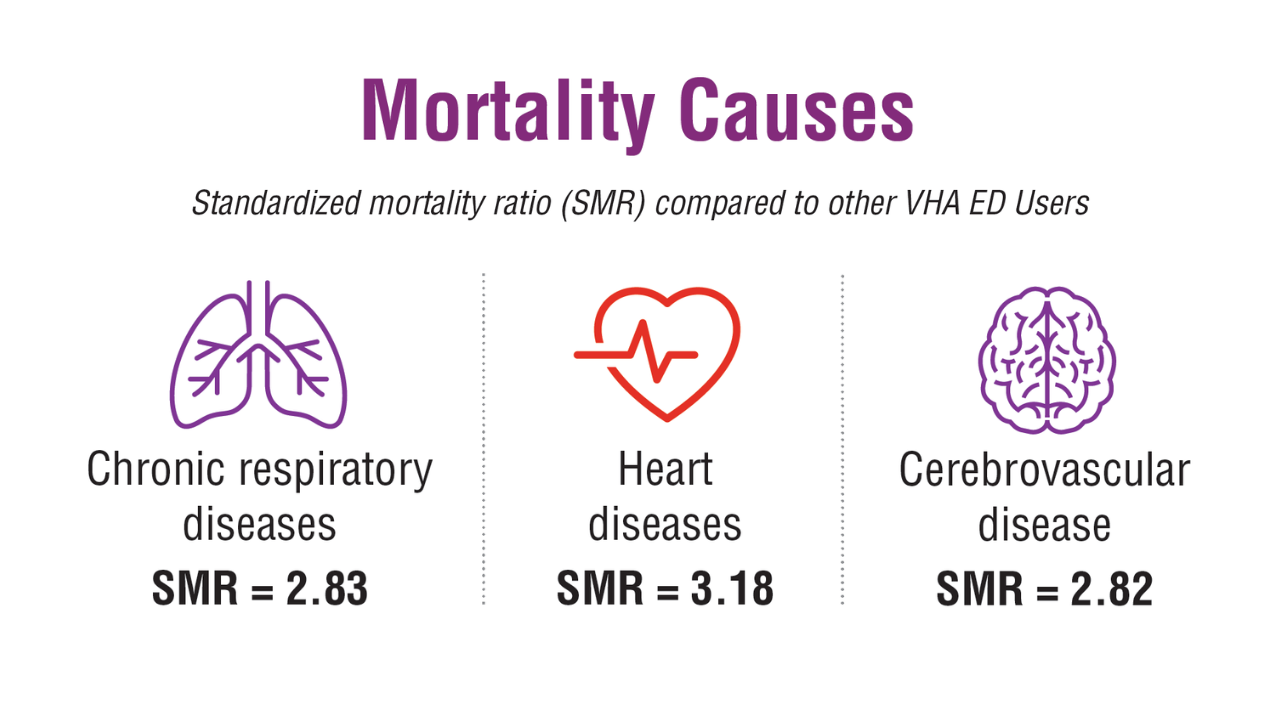 High-Risk ED Visits for Suicidality and Overdose4
High-Risk ED Visits for Suicidality and Overdose4
Patients with high-risk ED visits had increased mortality rates compared to other VHA ED users, other VHA users, and the US general population. This increase was highest in Asian or Pacific Islander and White veterans (SMR = 3.50, SMR = 3.11, respectively, compared to other VHA ED users).
Click to view more from Federal Health Care Data Trends 2025.
,false