AI-Based Risk Stratification for Oropharyngeal Carcinomas: AIROC





Vlad C. Sandulache, MD, PhD
Associate Professor;
Department of Otolaryngology,
Head and Neck Surgery
Baylor College of Medicine;
Staff Physician
Michael E. DeBakey VA Medical Center
Houston, Texas
Disclosures: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: FemtoVox Inc (Consultant; Equity holder); PDS Biotech (consultant).
Received income in an amount equal to or greater than $250 from: FemtoVox Inc; PDS Biotech.





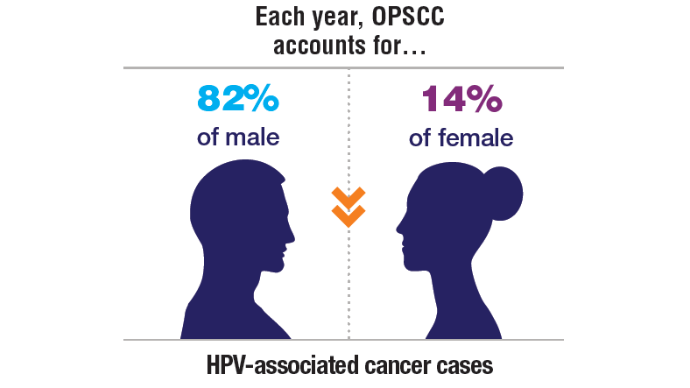
In recent years, human papillomavirus (HPV)-associated oropharyngeal squamous cell carcinoma (OPSCC) has been on the rise in the veteran population, where smoking rates (a contributor to OPSCC development) have historically been higher than in the general population.1 Variable treatment response rates and survival in patients with OPSCC indicate that whereas some patients may benefit from treatment de-escalation and a concomitant reduction in treatment-related adverse effects, aggressive disease in a subset of patients mandates the use of rigorous chemoradiation treatments.2,3 At present, effective stratification systems identifying these patient subsets are lacking.4
To address this clinical gap, a team of VA clinicians and researchers is developing AIROC (an artificial intelligence [AI]-based risk stratification algorithm for oropharyngeal carcinomas).a AIROC is an AI and machine learning (ML)-based algorithm that may successfully stratify veterans with HPV-associated OPSCC into risk categories that can enable safer de-escalation or escalation of cancer treatments.5-7 By integrating AIROC into clinical practice, the VHA aims to personalize cancer treatment, improve patient outcomes, and establish a new standard of care for veterans with this deadly disease.
aThis work is funded by the Veterans Affairs Clinical Science Research and Development (CSRD) Service (grant I01BX006380).
 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10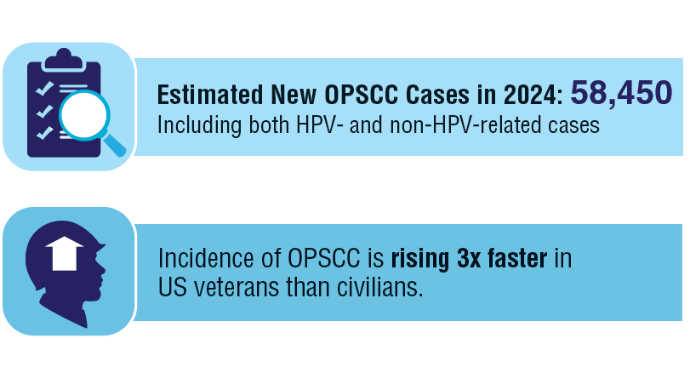 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10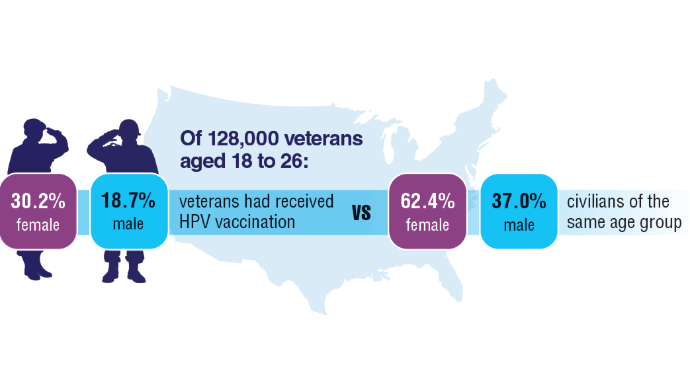 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10
HPV-associated cancers cause substantial clinical and economic burden to the VHA. There are no vaccination requirements or campaigns targeting the young veteran and active-duty populations. These low HPV vaccination rates will contribute to thousands of avoidable HPV-associated cancers and cancer-related deaths over the coming decades.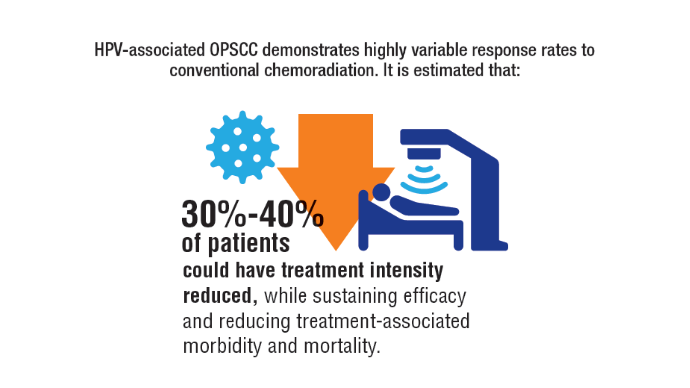 Modifying Treatment Intensity
Modifying Treatment Intensity
Current unselective approaches to de-escalation and escalation have not demonstrated success, generating a significant unmet clinical need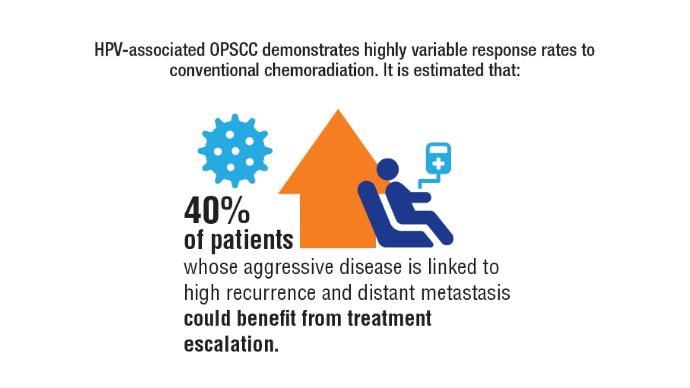 Modifying Treatment Intensity
Modifying Treatment Intensity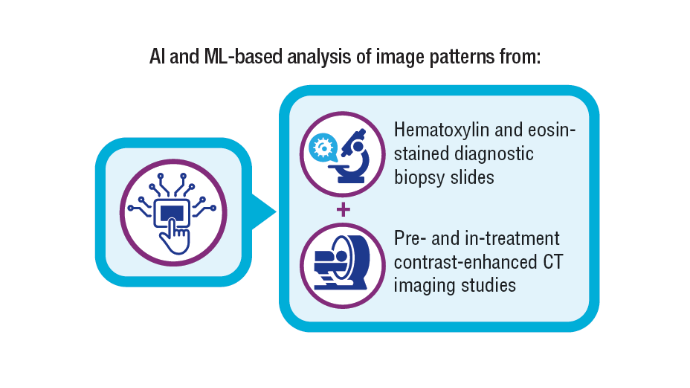 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13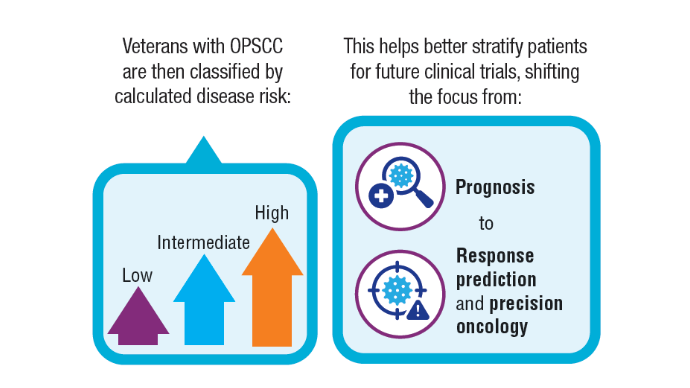 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13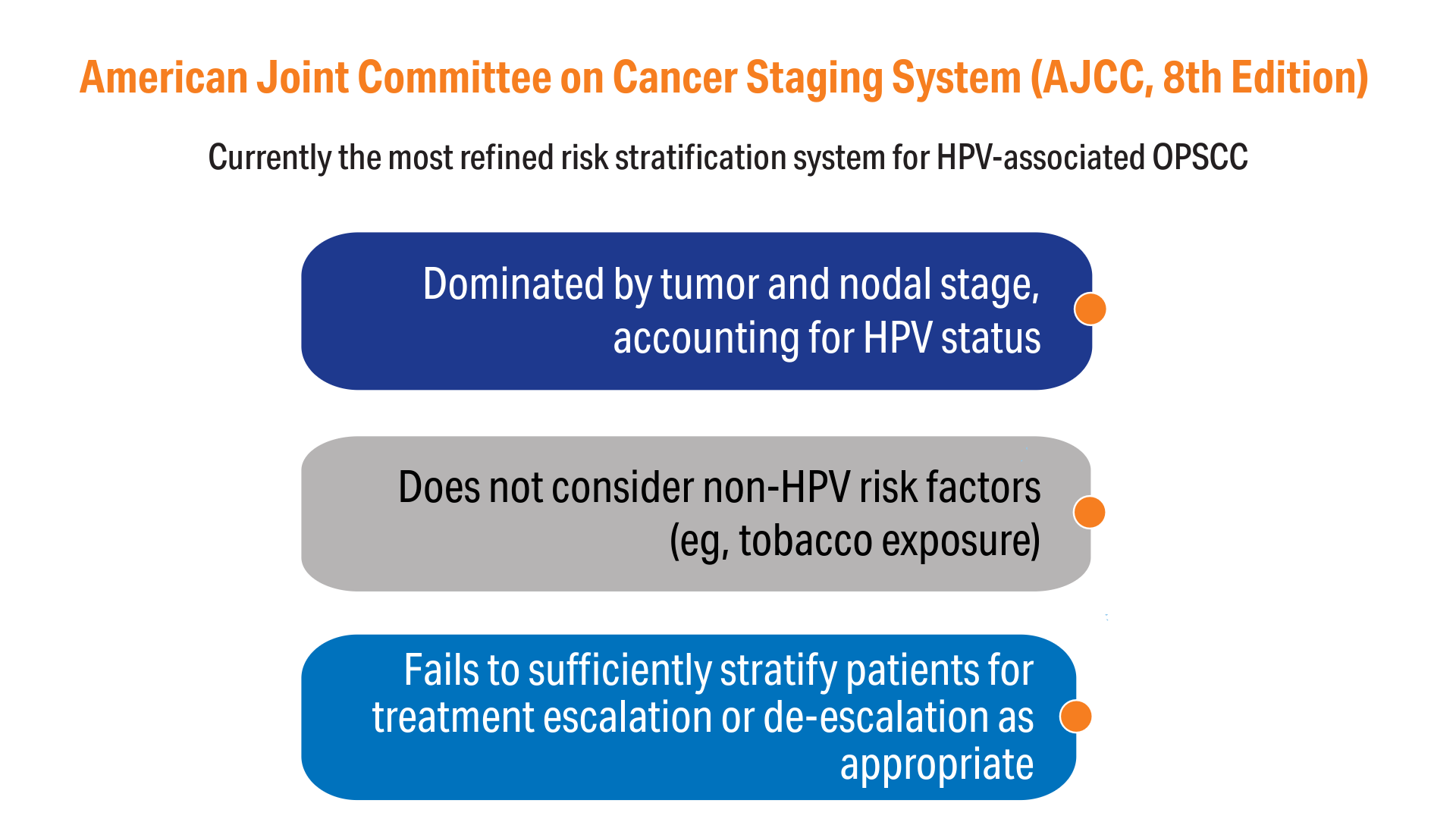 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13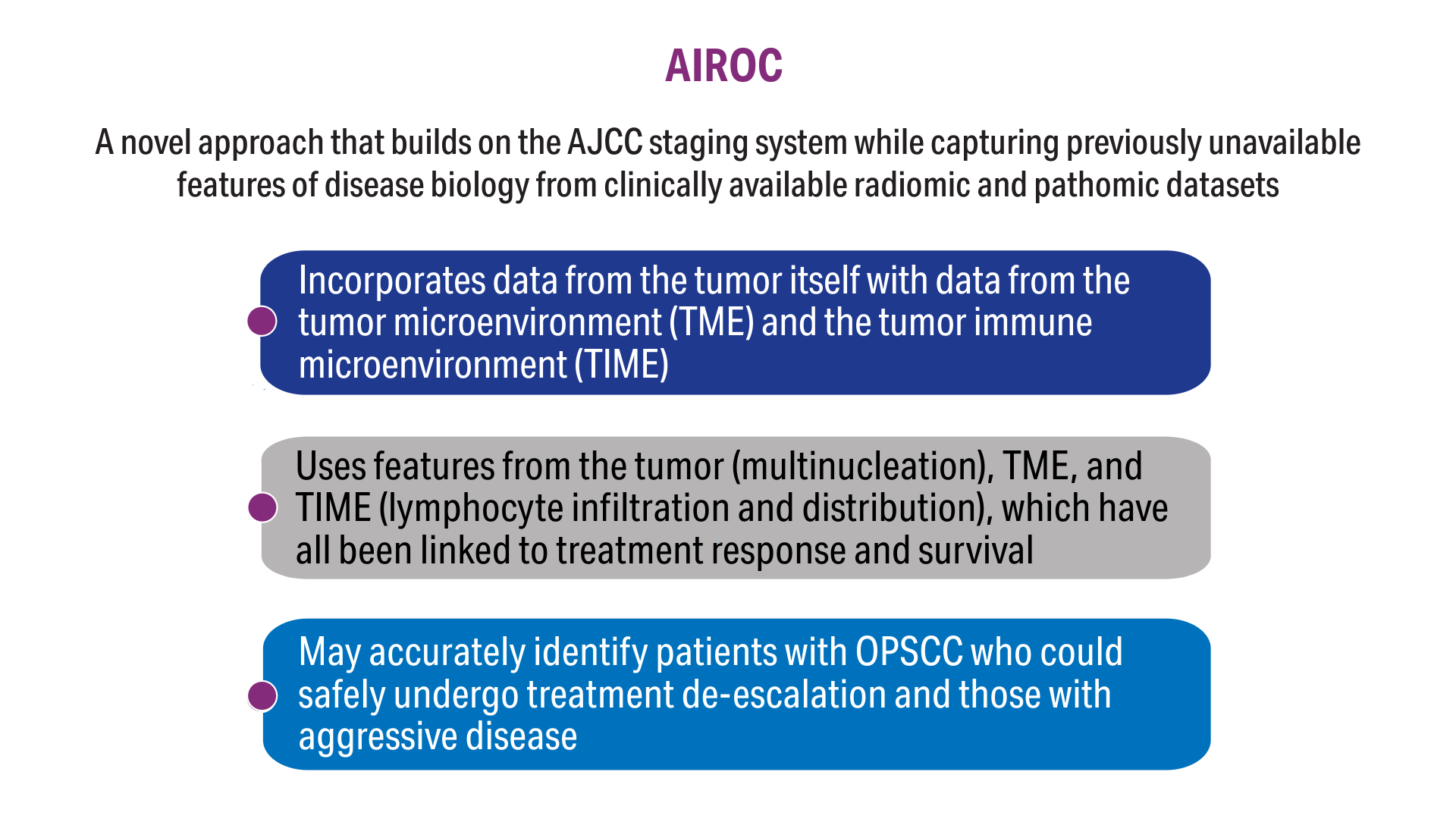 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13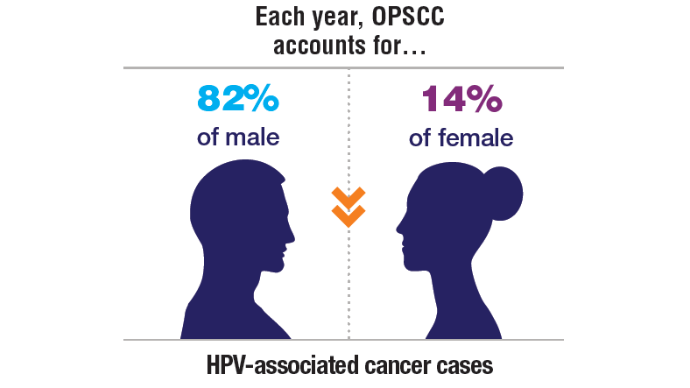 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10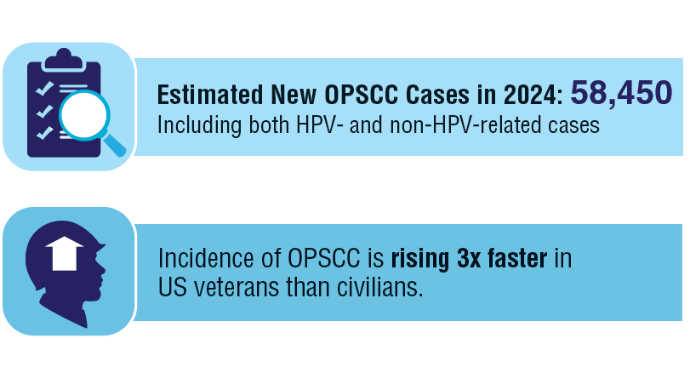 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10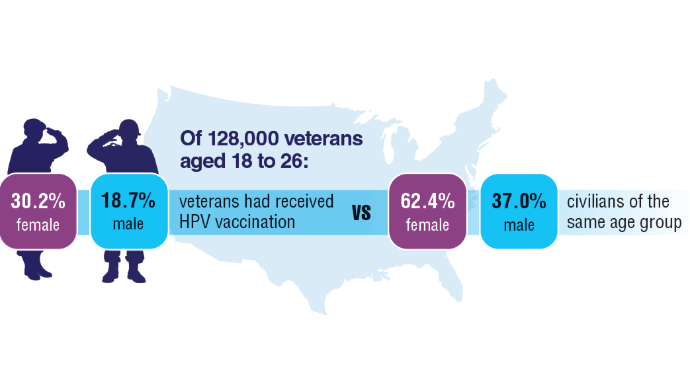 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10
HPV-associated cancers cause substantial clinical and economic burden to the VHA. There are no vaccination requirements or campaigns targeting the young veteran and active-duty populations. These low HPV vaccination rates will contribute to thousands of avoidable HPV-associated cancers and cancer-related deaths over the coming decades.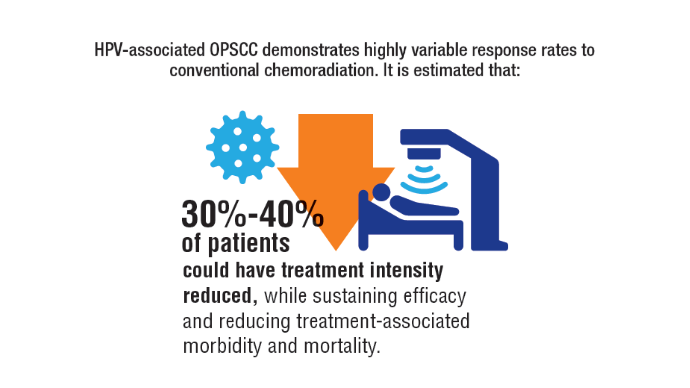 Modifying Treatment Intensity
Modifying Treatment Intensity
Current unselective approaches to de-escalation and escalation have not demonstrated success, generating a significant unmet clinical need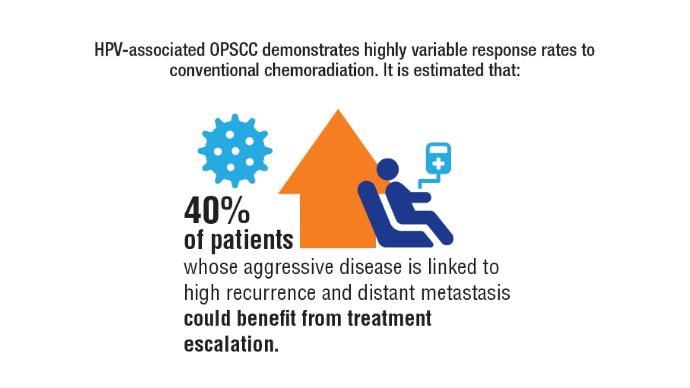 Modifying Treatment Intensity
Modifying Treatment Intensity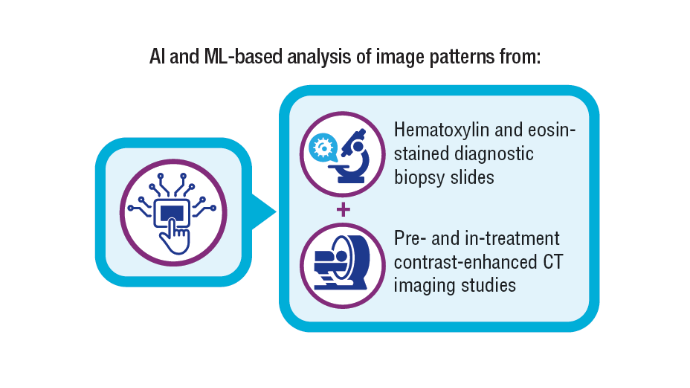 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13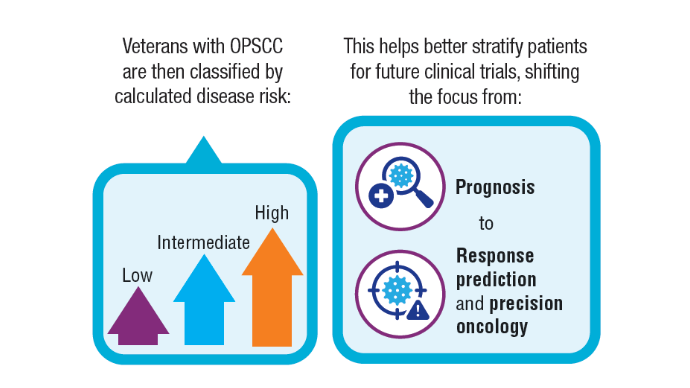 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13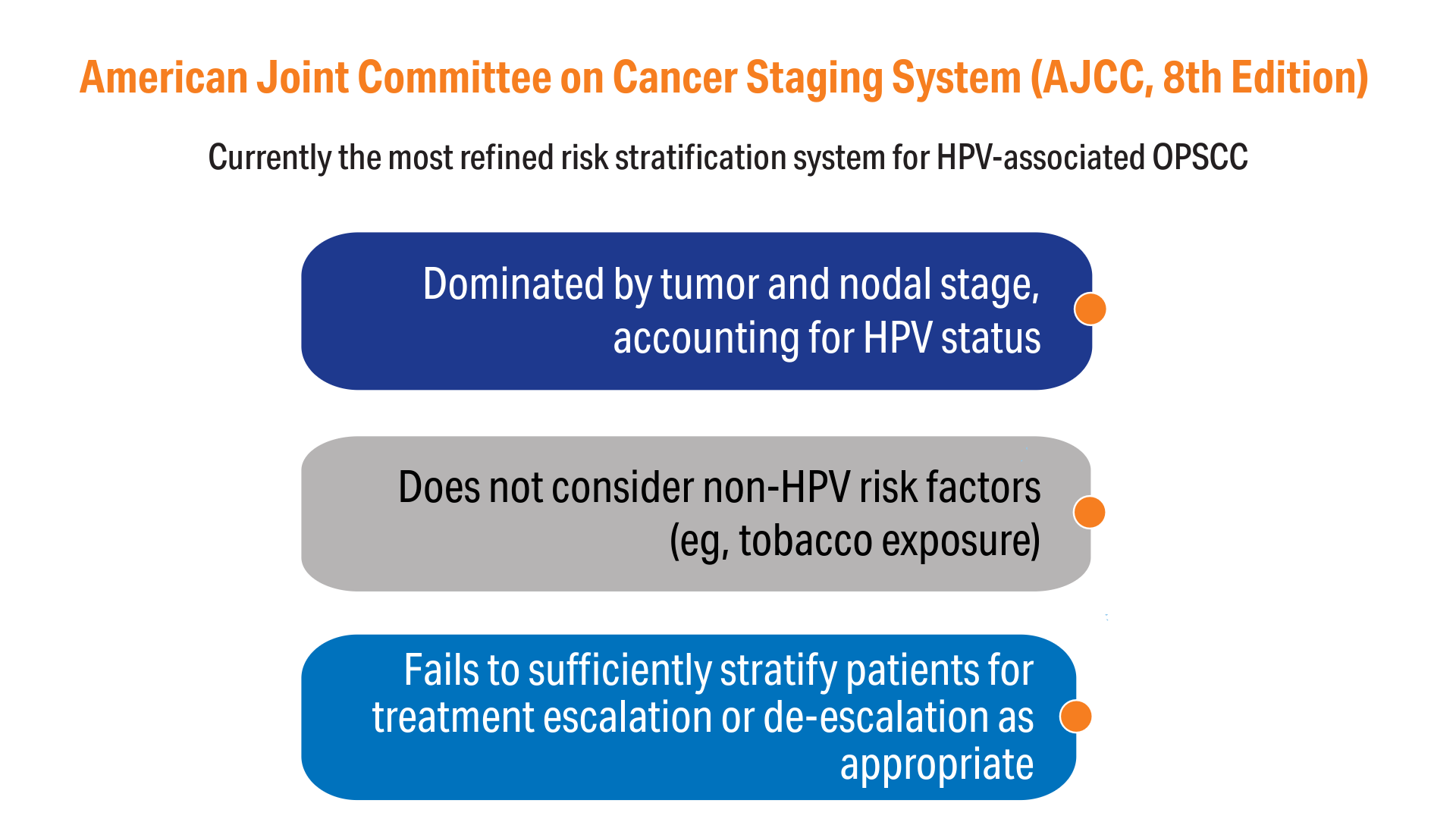 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13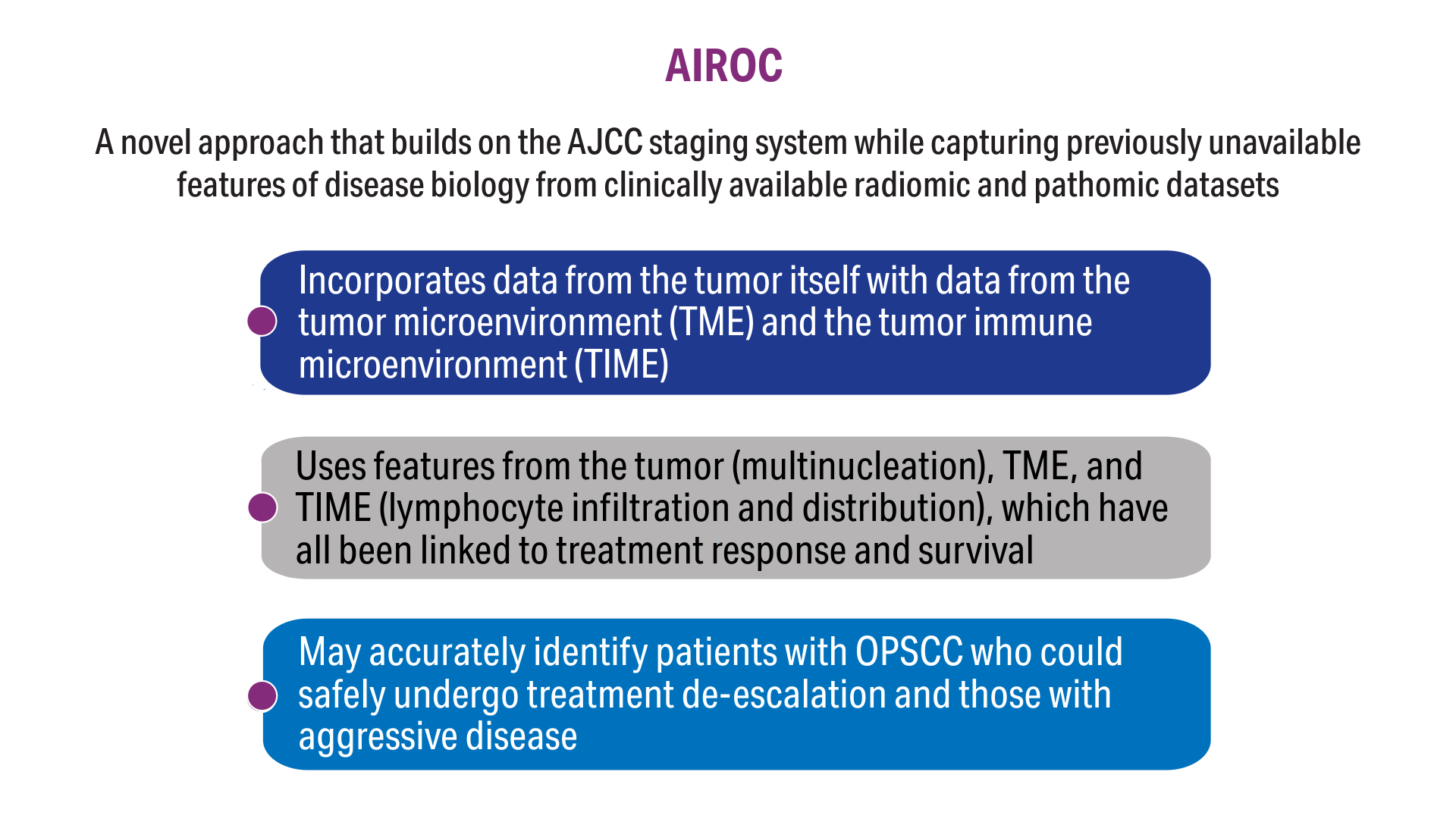 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13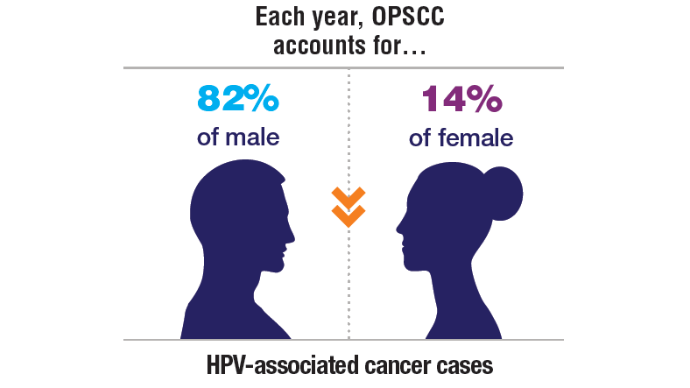 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10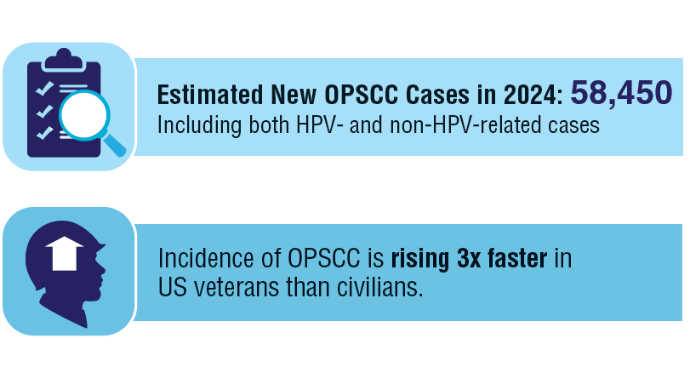 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10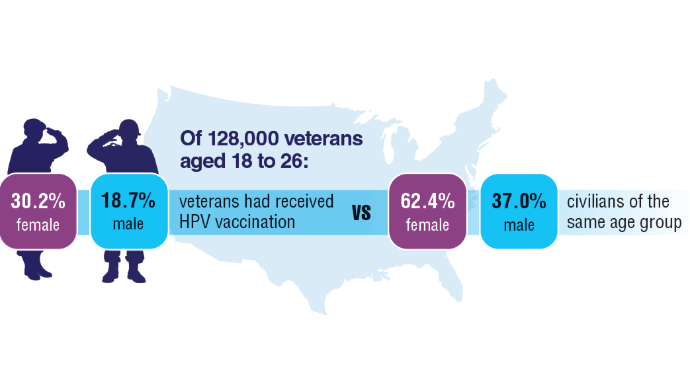 A Clinical Problem in the United States1,8-10
A Clinical Problem in the United States1,8-10
HPV-associated cancers cause substantial clinical and economic burden to the VHA. There are no vaccination requirements or campaigns targeting the young veteran and active-duty populations. These low HPV vaccination rates will contribute to thousands of avoidable HPV-associated cancers and cancer-related deaths over the coming decades.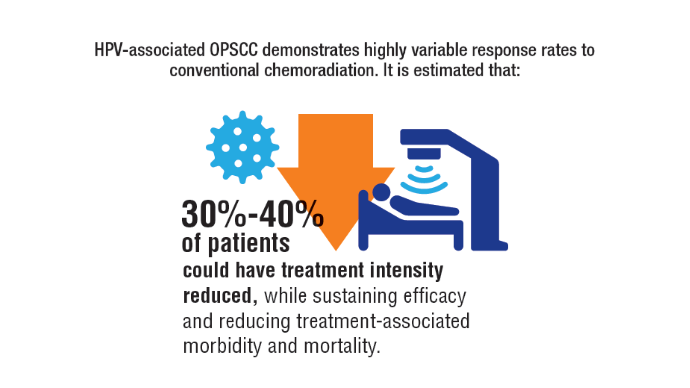 Modifying Treatment Intensity
Modifying Treatment Intensity
Current unselective approaches to de-escalation and escalation have not demonstrated success, generating a significant unmet clinical need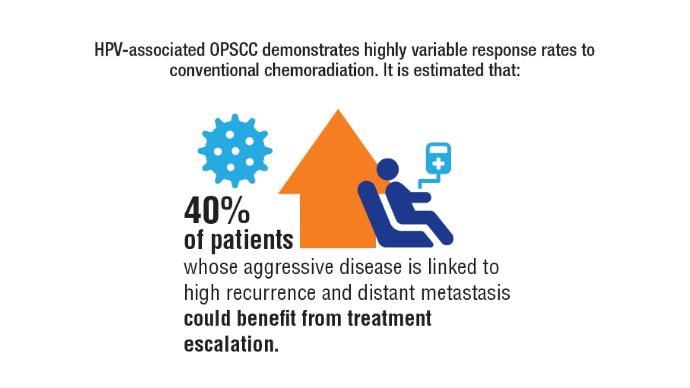 Modifying Treatment Intensity
Modifying Treatment Intensity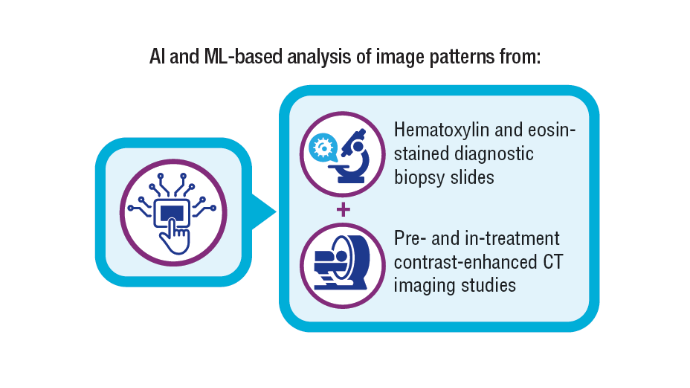 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13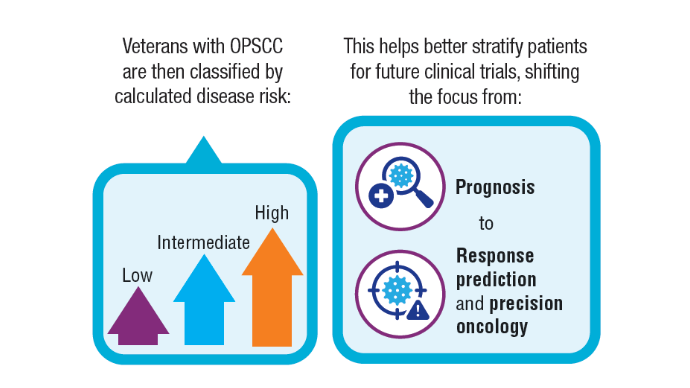 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13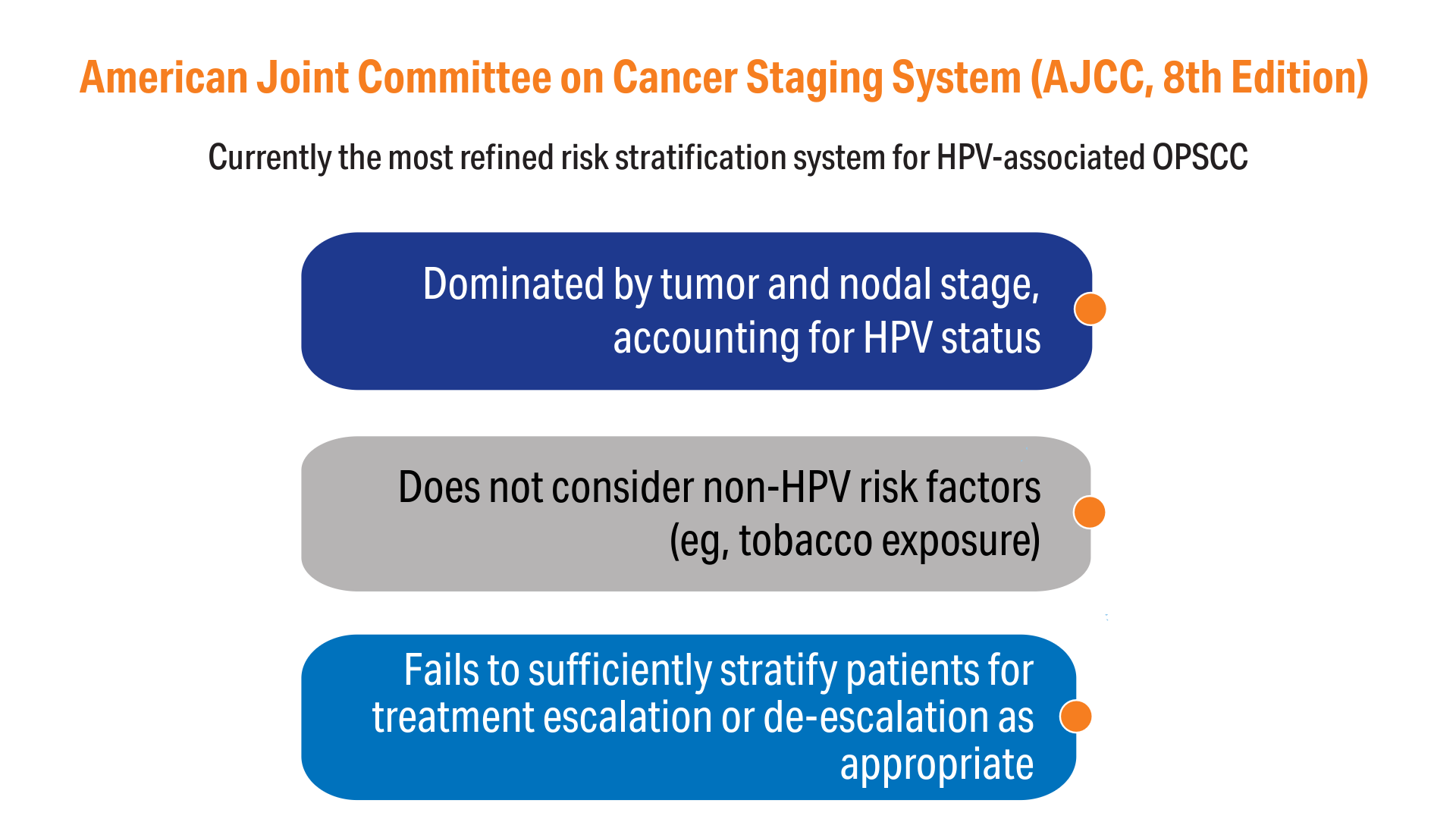 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13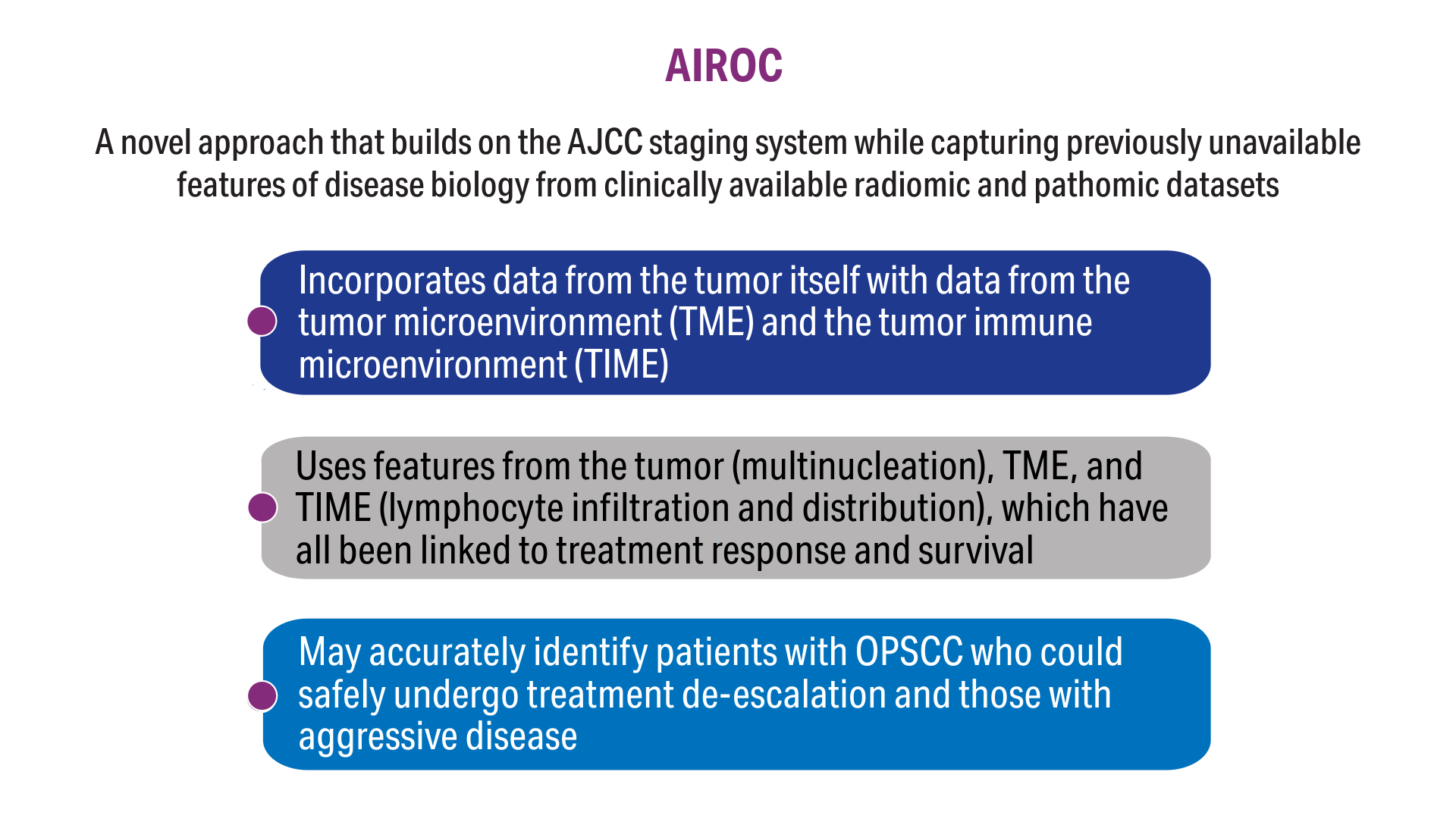 AIROC: Objectives and Innovation4,11-13
AIROC: Objectives and Innovation4,11-13
Click here to view more from Cancer Data Trends 2025.
,false