Lung Cancer: Mortality Trends in Veterans and New Treatments





Mille Das, MD
Clinical Professor
Department of Medicine/Oncology
Stanford University
Stanford, California;
Chief, Oncology
Department of Medicine
VA Palo Alto Health Care System
Palo Alto, California
Disclosures: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Sanofi/ Genzyme; Regeneron; Janssen; Astra Zeneca; Gilead; Bristol Myer Squibb; Catalyst Pharmaceuticals; Guardant; Novocure; AbbVie; Daiichi Sankyo.
Received research grant from: Merck; Genentech; CellSight; Novartis; Varian.
Received income in an amount equal to or greater than $250 from: Plexus; IDEO; Springer; Medical Educator Consortium; Dedham Group; DAVA Oncology; MJH Healthcare Holdings; Targeted Oncology; OncLive; ANCO; Aptitude Health; MashUp Media; Med Learning Group; Curio; Triptych Health; American Cancer Society.





The annual incidence rate of lung cancer among veterans is substantial and increasing, tripling from 2000 to 2017; historically, it was largely due to higher rates of smoking.1 In recent years, the VHA has aimed to improve survival rates of patients with lung cancer across all disease stages and racial/ethnic groups.2 These efforts include providing increased screening, molecular testing, and access to targeted therapies; adopting advanced surgical and biopsy techniques; and implementing nurse navigators to guide care.2
Veterans often have lung cancers that are strongly associated with smoking, which are less likely to harbor specific driver mutations such as EGFR or ALK alterations. This can limit the use of targeted therapies specifically designed for these mutations.1,3 However, newly developed immunotherapy agents, which do not rely on the presence of driver mutations, have shown significant efficacy in patients with non-small cell lung cancer (NSCLC), particularly in cases with high PD-L1 expression.4-6
 3-Year Overall Survival Trends in Veterans2
3-Year Overall Survival Trends in Veterans2
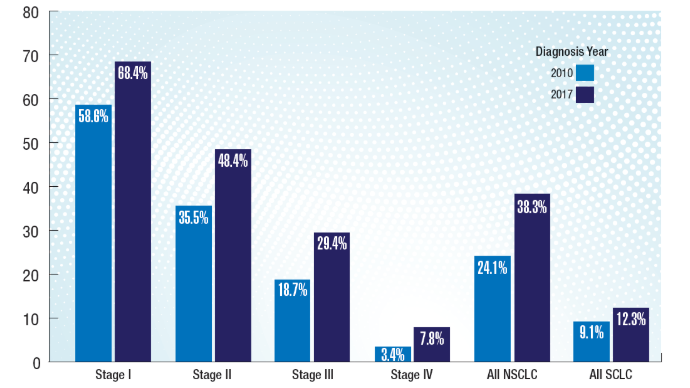
A 2024 study of more than 50,000 veterans with lung cancer diagnosed through the VHA demonstrated improved survival trends regardless of disease stage or type of lung cancer (NSCLC or small cell lung cancer [SCLC]). This finding could be due in part to an observed 68% increase in stage I diagnoses and 11% decrease in stage IV diagnoses, underscoring the positive impact of increased screening and early detection.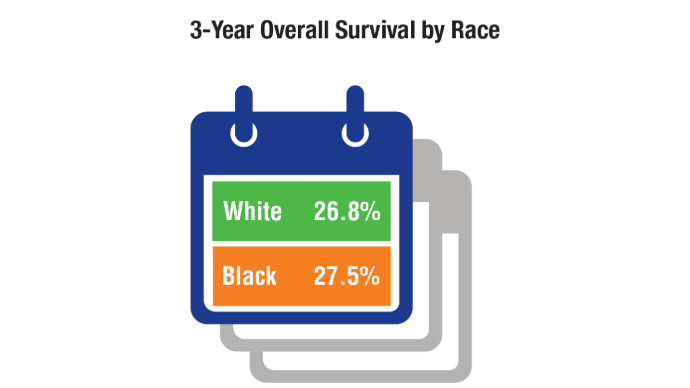 Survival Trends by Race in Veterans2
Survival Trends by Race in Veterans2
Black veterans had slightly higher lung cancer survival rates, which could be due to equity policy interventions in the VHA compared to those in other health care systems.2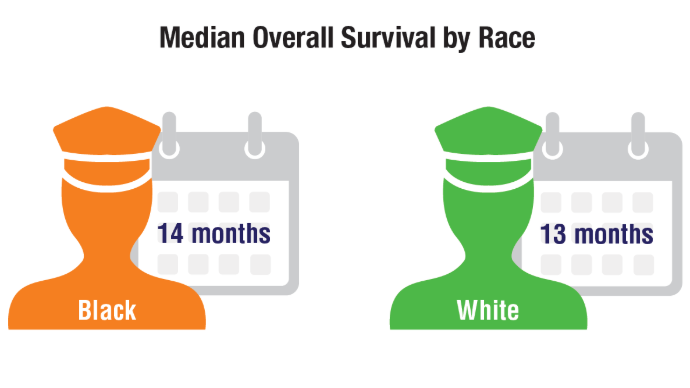 Survival Trends by Race in Veterans2
Survival Trends by Race in Veterans2
Black veterans also had higher overall survival specifically for SCLC when subtypes were compared. These trends differ from national trends outside the VA, which usually show worse outcomes for Black patients.7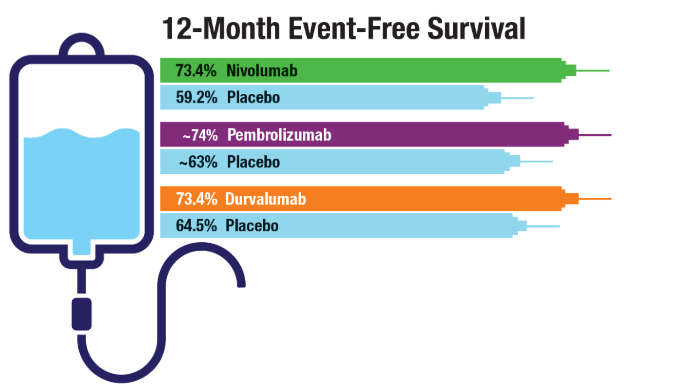 Immunotherapy in Resectable NSCLC4-6
Immunotherapy in Resectable NSCLC4-6
Immune checkpoint inhibitors, such as nivolumab, pembrolizumab, and durvalumab, have demonstrated efficacy in patients with early-stage resectable NSCLC, and their use should be considered in eligible veterans. In particular, the perioperative trials have indicated higher rates of complete pathological response (defined as ≤ 10% residual viable tumor cells in the primary tumor after surgery). For example, nivolumab showed a 25.3% complete pathological response compared to 4.7% with placebo and higher rates of event-free survival among patients receiving immunotherapy as part of neoadjuvant and adjuvant treatment vs chemotherapy alone. All groups received neoadjuvant chemotherapy in addition to either immunotherapy or placebo. Adjuvant therapy consisted of an immunotherapy agent or placebo.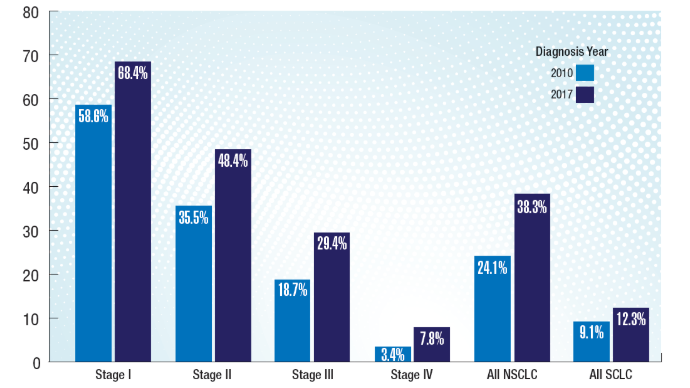 3-Year Overall Survival Trends in Veterans2
3-Year Overall Survival Trends in Veterans2
A 2024 study of more than 50,000 veterans with lung cancer diagnosed through the VHA demonstrated improved survival trends regardless of disease stage or type of lung cancer (NSCLC or small cell lung cancer [SCLC]). This finding could be due in part to an observed 68% increase in stage I diagnoses and 11% decrease in stage IV diagnoses, underscoring the positive impact of increased screening and early detection.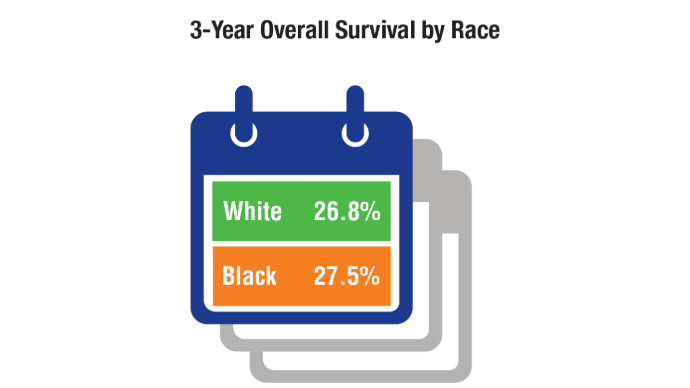 Survival Trends by Race in Veterans2
Survival Trends by Race in Veterans2
Black veterans had slightly higher lung cancer survival rates, which could be due to equity policy interventions in the VHA compared to those in other health care systems.2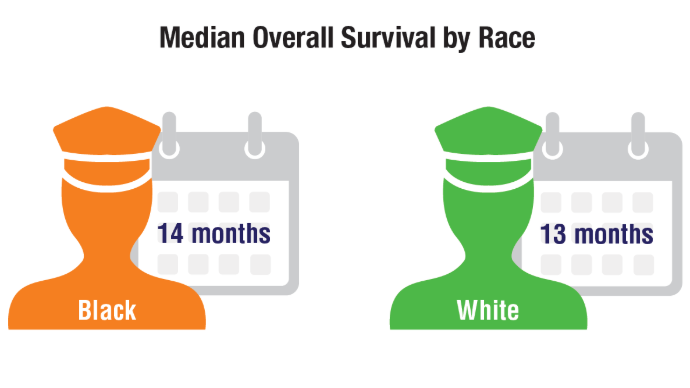 Survival Trends by Race in Veterans2
Survival Trends by Race in Veterans2
Black veterans also had higher overall survival specifically for SCLC when subtypes were compared. These trends differ from national trends outside the VA, which usually show worse outcomes for Black patients.7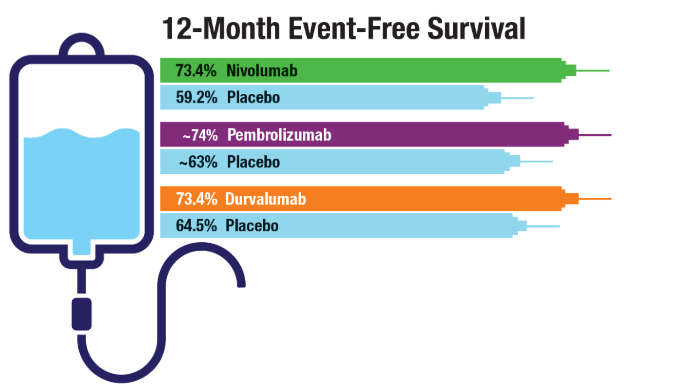 Immunotherapy in Resectable NSCLC4-6
Immunotherapy in Resectable NSCLC4-6
Immune checkpoint inhibitors, such as nivolumab, pembrolizumab, and durvalumab, have demonstrated efficacy in patients with early-stage resectable NSCLC, and their use should be considered in eligible veterans. In particular, the perioperative trials have indicated higher rates of complete pathological response (defined as ≤ 10% residual viable tumor cells in the primary tumor after surgery). For example, nivolumab showed a 25.3% complete pathological response compared to 4.7% with placebo and higher rates of event-free survival among patients receiving immunotherapy as part of neoadjuvant and adjuvant treatment vs chemotherapy alone. All groups received neoadjuvant chemotherapy in addition to either immunotherapy or placebo. Adjuvant therapy consisted of an immunotherapy agent or placebo.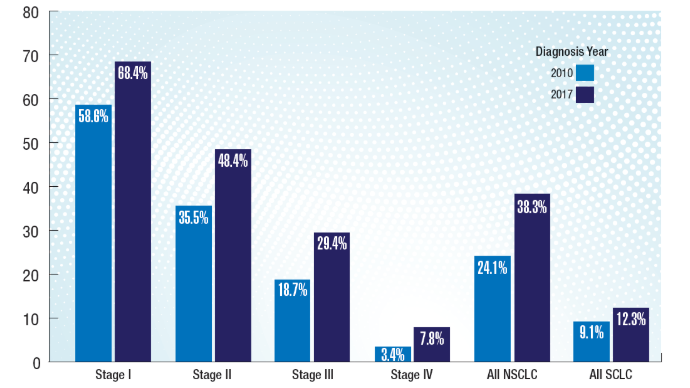 3-Year Overall Survival Trends in Veterans2
3-Year Overall Survival Trends in Veterans2
A 2024 study of more than 50,000 veterans with lung cancer diagnosed through the VHA demonstrated improved survival trends regardless of disease stage or type of lung cancer (NSCLC or small cell lung cancer [SCLC]). This finding could be due in part to an observed 68% increase in stage I diagnoses and 11% decrease in stage IV diagnoses, underscoring the positive impact of increased screening and early detection.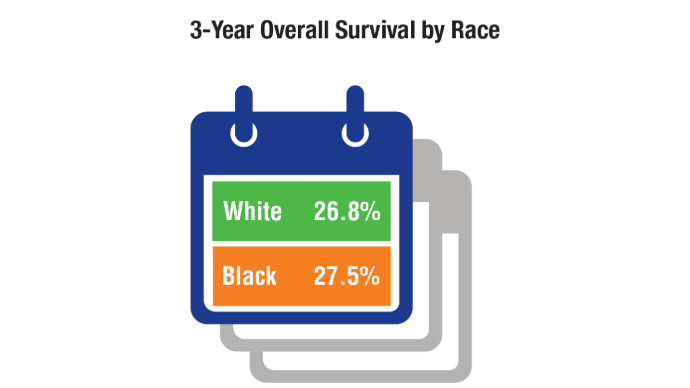 Survival Trends by Race in Veterans2
Survival Trends by Race in Veterans2
Black veterans had slightly higher lung cancer survival rates, which could be due to equity policy interventions in the VHA compared to those in other health care systems.2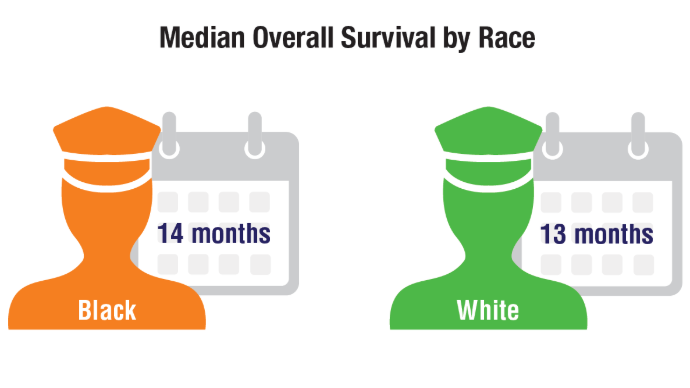 Survival Trends by Race in Veterans2
Survival Trends by Race in Veterans2
Black veterans also had higher overall survival specifically for SCLC when subtypes were compared. These trends differ from national trends outside the VA, which usually show worse outcomes for Black patients.7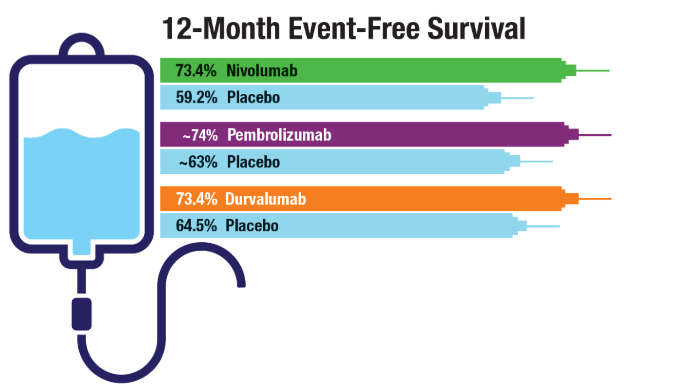 Immunotherapy in Resectable NSCLC4-6
Immunotherapy in Resectable NSCLC4-6
Immune checkpoint inhibitors, such as nivolumab, pembrolizumab, and durvalumab, have demonstrated efficacy in patients with early-stage resectable NSCLC, and their use should be considered in eligible veterans. In particular, the perioperative trials have indicated higher rates of complete pathological response (defined as ≤ 10% residual viable tumor cells in the primary tumor after surgery). For example, nivolumab showed a 25.3% complete pathological response compared to 4.7% with placebo and higher rates of event-free survival among patients receiving immunotherapy as part of neoadjuvant and adjuvant treatment vs chemotherapy alone. All groups received neoadjuvant chemotherapy in addition to either immunotherapy or placebo. Adjuvant therapy consisted of an immunotherapy agent or placebo.
Click to view more from Cancer Data Trends 2025.
,false