Data Trends 2023: Rheumatoid Arthritis










Slideshow below.
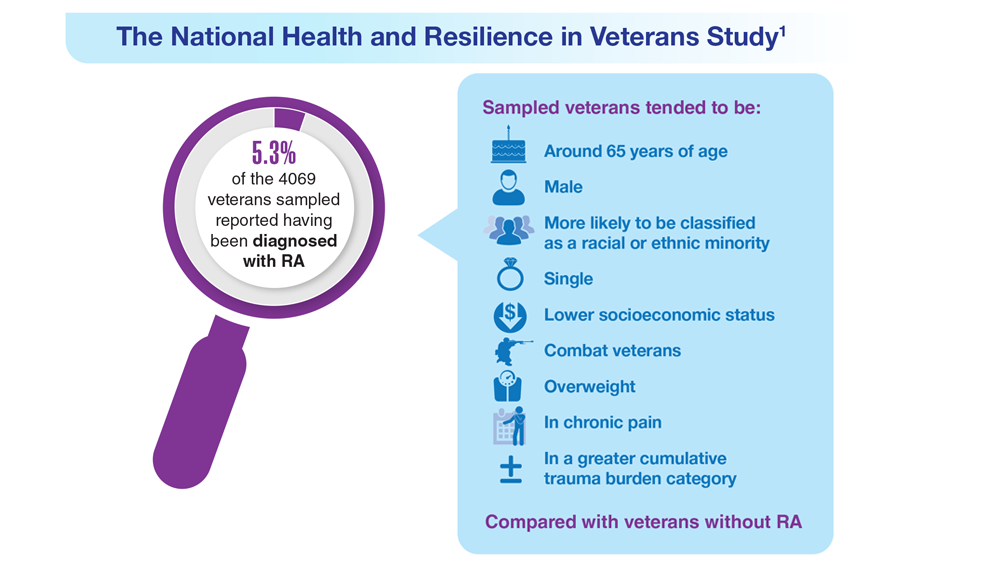
One in 20 veterans have been diagnosed with rheumatoid arthritis (RA). It is more common among certain sociodemographic groups and has been associated with an enhanced mental and physical health burden.1
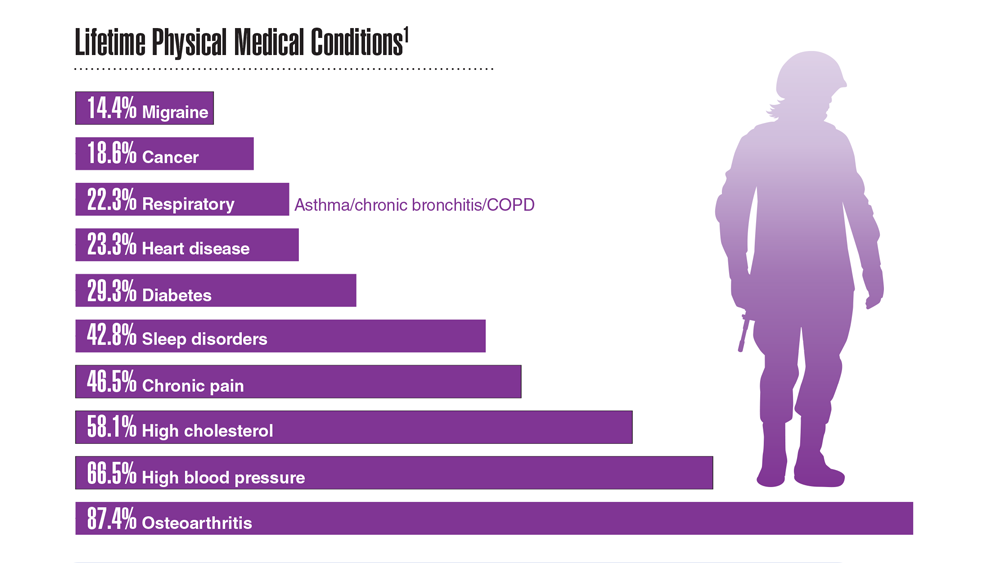
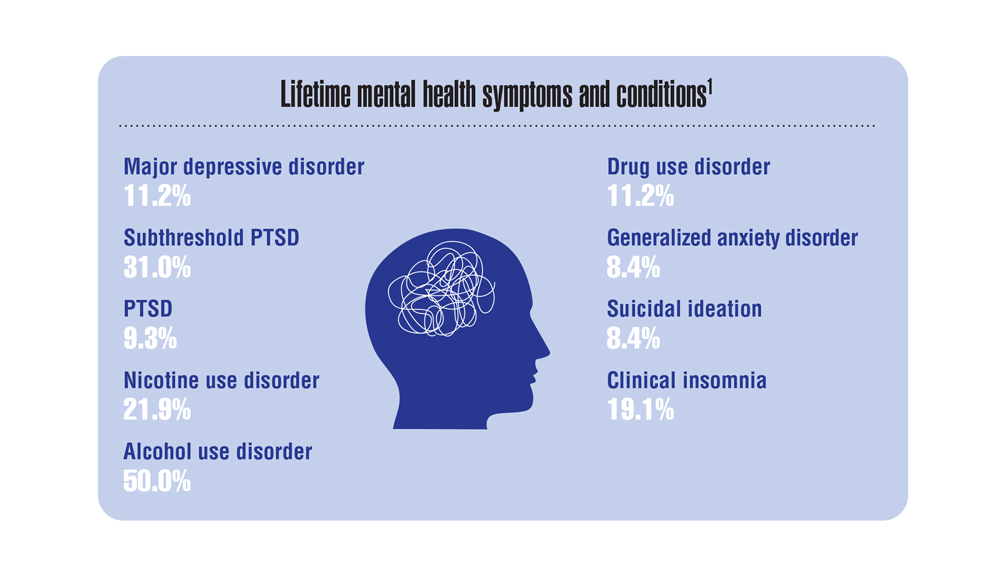
The 2019-2020 National Health and Resilience in Veterans Study (NHRVS) showed that RA in the veteran population is associated with several comorbid medical conditions, more severe somatic symptoms, higher occurrence of insomnia, subthreshold PTSD, and increased alcohol use.1
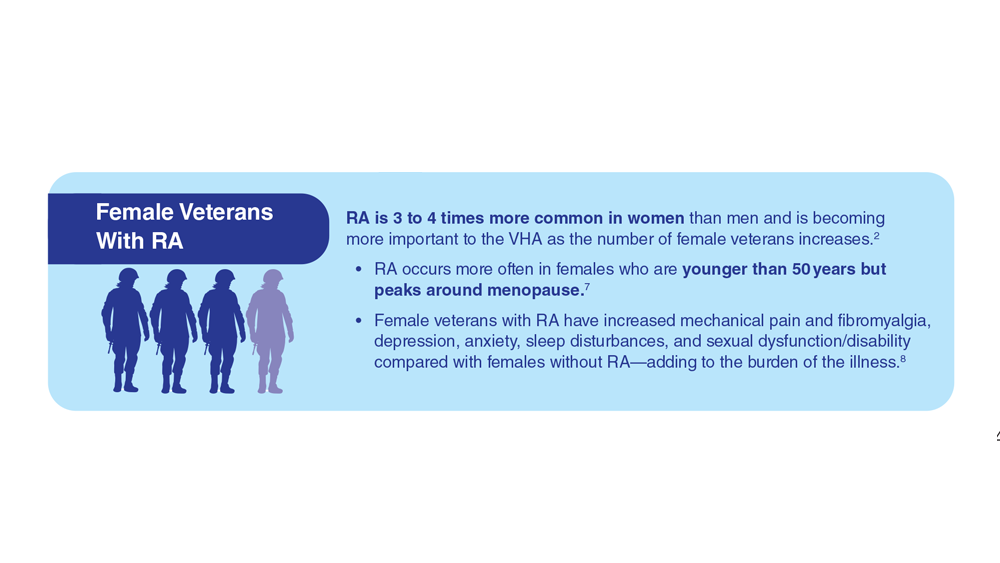
RA is 3 times more common in people assigned as female at birth compared with people assigned as male.2 Even though men currently comprise about 90% of the veteran population, the relevance of RA to the VA health system has grown with the continued increase in female veterans.3
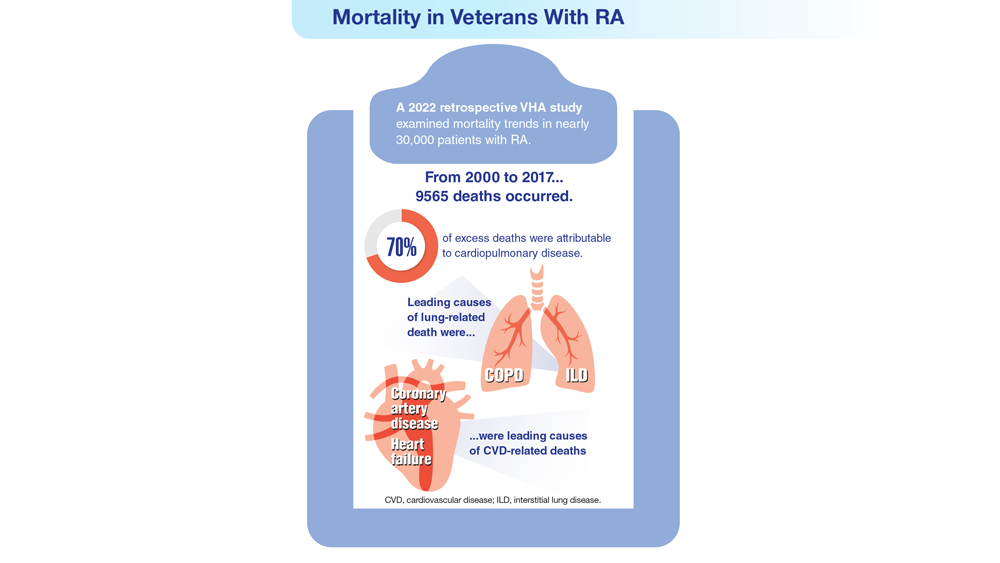
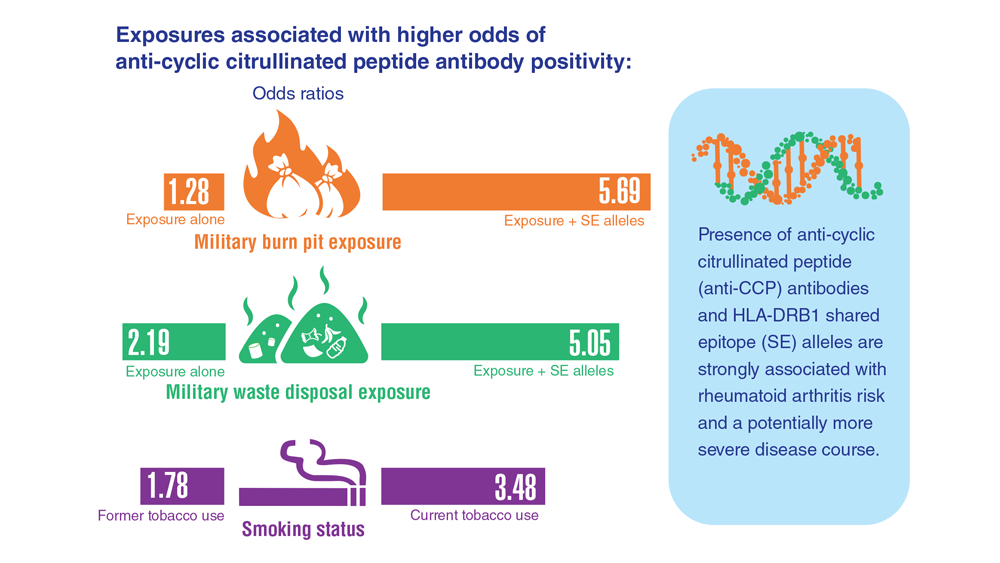
A retrospective study of VHA records from the past 2 decades examined temporal trends in all-cause and cause-specific mortality in patients with RA. Excess RA-related mortality was shown to be driven by cardiovascular, cancer, respiratory, and infectious causes—particularly cardiopulmonary diseases.4 Findings have also suggested that military burn pit and waste disposal inhalant exposures are associated with autoantibody expression in RA, possibly affecting the risk of developing RA and the disease course itself.5 These findings support the predictor that not only lung disease but also smoking is a major driver of RA disease state.6