Lung Cancer Screening in Veterans





Apar Kishor Ganti, MD, MS
Doctor and Mrs. D. Leon UNMC Research
Fund Chair in Internal Medicine
Staff Physician, VA Nebraska-Western Iowa Health Care System
Professor of Medicine, Division of Oncology-Hematology
Professor (Courtesy) of Biochemistry and Molecular Biology
Associate Director of Clinical Research, Fred & Pamela Buffett Cancer Center
University of Nebraska Medical Center
Omaha, NE





Slideshow below.
In the United States and among veterans, lung cancer has the highest rate of cancer-related mortality. Earlier detection and increased screening of high-risk individuals can improve the overall survival rate.1 With the broadening of the USPSTF lung cancer screening guidelines, in 2020 an estimated 15 million people in the United States—including at least 900,000 veterans—were eligible for lung cancer screening by CT.2,3 However, only 5% of those eligible were screened.4,5 One reason for this vast discrepancy is uneven access. Estimates in 2021 were that <20% of eligible veterans have undergone lung cancer screening because of problems accessing it in rural areas.6
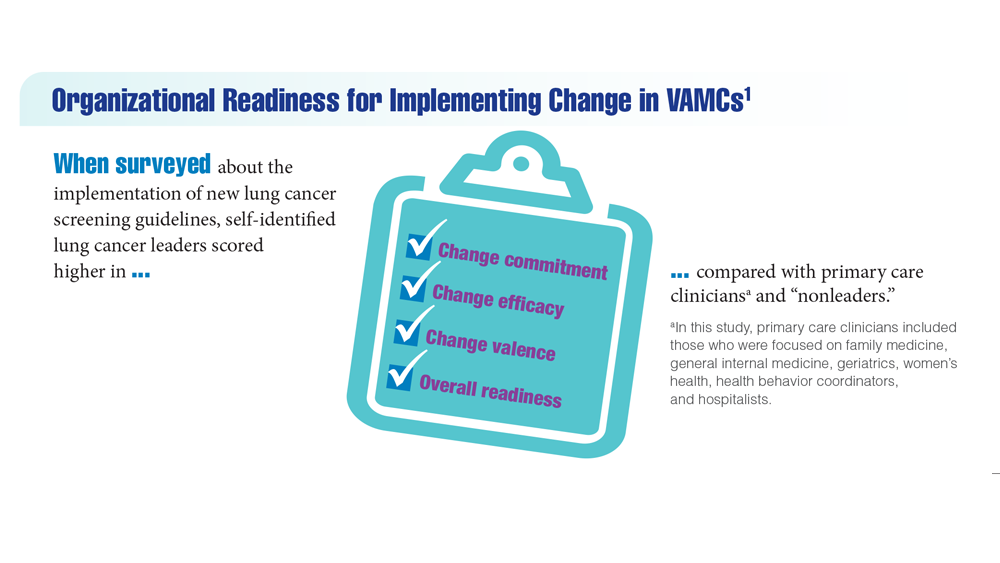
Implementing the expanded USPSTF guidelines is key to maximizing screening among underserved populations, such as those in rural areas who may lack access to nearby health care, as well as racial and ethnic minorities.1 A study of one VAMCs standardization of screening practices found that radiologists were more likely to adapt to these changes than primary care clinicians, suggesting a need to better understand differences in health care professional practices and priorities to universally improve screening rates across the VA.1
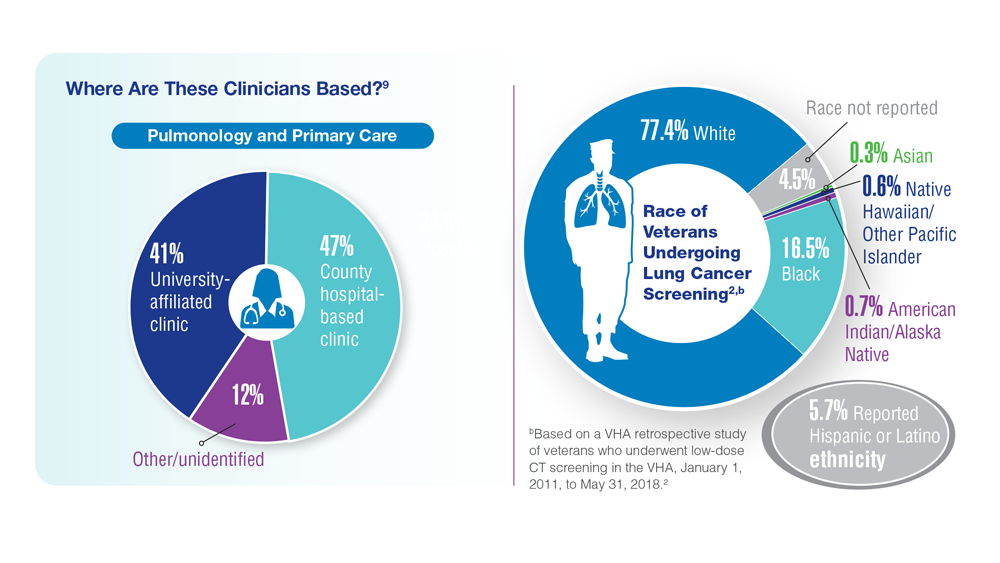
An important question will always be how many high-risk veterans are being screened for lung cancer?1 To ensure proper care, it is important to understand the characteristics of clinicians who provide screening based on setting and clinical areas of expertise. Where are they, who are they, and how do our most vulnerable populations gain access? Access is critical, particularly among clinicians who typically provide screening to those underserved populations.
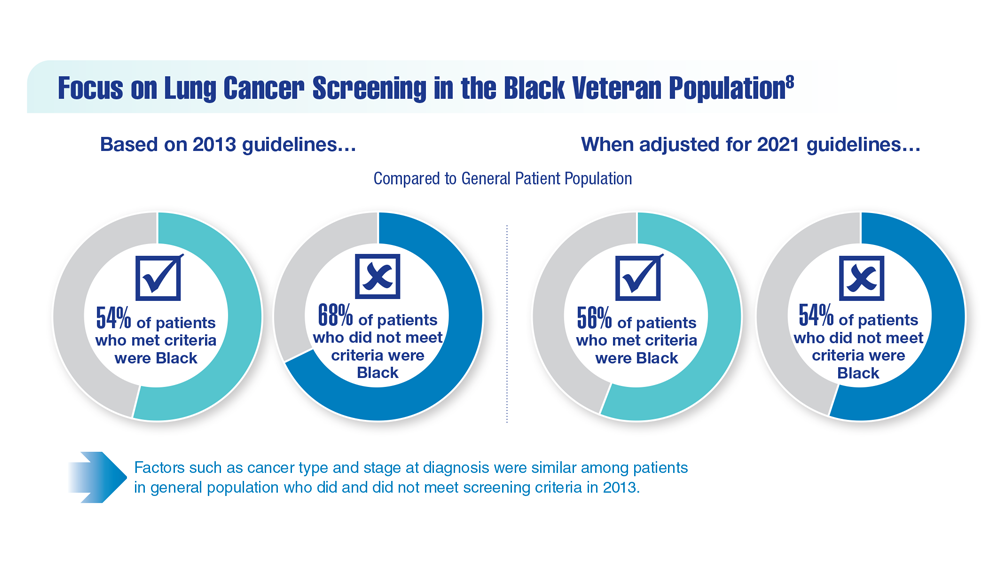
Although lung cancer screening rates have increased over the years, overall, utilization remains low, even though data show a 20% reduction in lung cancer mortality with adherence to yearly CT screening.7 Looking at these rates helps us understand the need to intervene to increase lung cancer screening rates.8 Guidelines have been an essential component when it comes to outcomes related to screenings. Through programs implemented by the VHA, the goal is to improve the uptake and quality of lung cancer screening and optimize the practice and access for all veterans.9 For clinicians, future work should evaluate lung cancer screening programs with high vs low rates of adherence to identify and publicize best practices for timely, appropriate follow-up.9 Although adherence rates remain low regardless of race, further research, particularly among Black veterans, is encouraged to address delayed follow-up and to create culturally competent and inclusive lung cancer screening programs.10