Strategies for improved management of hypothyroidism
Management is clear-cut—yet many patients don’t reach treatment goals. To optimize quality of life, master the fine points of T4 replacement and address the impact of comorbidities.
PRACTICE RECOMMENDATIONS
› Prescribe levothyroxine (LT4) to maintain thyroid-stimulating hormone (TSH) at 4 to 7 mIU/L in select patients with primary hypothyroidism for whom that range of the serum TSH level can be considered appropriate (ie, those older than 65 years and those who have underlying coronary artery disease or another debilitating chronic disorder). A
› Counsel all women of childbearing age with primary hypothyroidism that they need to have their dosage of LT4 increased as soon as pregnancy is suspected. A
› Keep in mind that treating hypothyroidism is not always necessary in older patients who have subclinical disease and a serum TSH level < 10 mIU/L. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Monitoring and titrating. Hypothyroid symptoms usually improve after 2 or 3 weeks of LT4 treatment; in severe hypothyroidism, complete recovery might take months. Approximately 6 weeks after LT4 therapy is initiated, serum TSH should be measured. After assessing whether administration of LT4 at the starting dosage is appropriate, that dosage can be increased, or decreased, every 4 to 6 weeks until the TSH goal is reached. Once the patient is maintained at a given dosage, measure serum TSH once a year—more often if there is an abnormal result or a change in the patient’s health status.23
Adverse effects of LT4 therapy are rare, unless over-replacement occurs. Rarely, patients have an allergy to the dye or an excipient (filler) in the tablet.26-28 The white, 50-mcg tablets can be given safely to patients with dye sensitivity. For those who have an allergy to an excipient (except gelatin) or gluten intolerance, the LT4 soft-gel capsule or liquid preparation (Tirosint) can be prescribed.
Pure LT4, in a capsule made from vegetable sources, can be ordered through a compounding pharmacy for patients who are allergic to animal products.
Anemia, especially iron-deficiency anemia, can cause intolerance to LT4 therapy; in such patients, lowering the starting dosage and treating anemia are indicated.29
Persistent symptoms (despite a normal TSH level). Because many hypothyroid symptoms are nonspecific, patients might come to think that their LT4 dosage is inadequate if they feel tired or gain weight. Persistent hypothyroid symptoms despite a normal serum TSH level might be due to (1) the inability of LT4 therapy to restore tissue thyroid hormone levels to normal or (2) other variables unrelated to hypothyroidism, including disorders associated with inflammation or autoimmune disease, certain medications, diet, lifestyle, and environmental toxins.
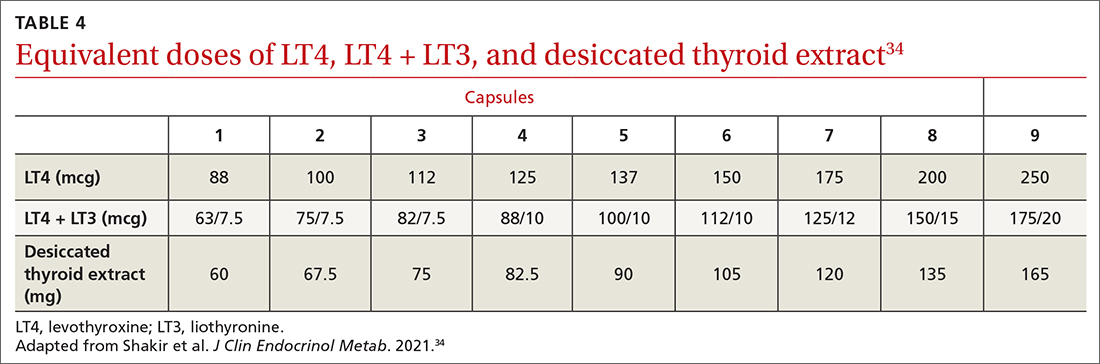
These patients might benefit from a detailed history to identify other causes and a switch to either LT4 + liothyronine (LT3; synthetic T3) combination therapy or DTE26,30-33 (TABLE 434), although a beneficial effect of LT4 + LT3 therapy was not seen in several studies.35,36 Over-replacement with LT4 should be discouraged, due to concerns about thyrotoxicosis and its complications (eg, atrial fibrillation, accelerated bone loss).
DTE and LT4 + LT3. Use of DTE has decreased since the 1970s, when LT4 became the therapy of choice. Subsequently, anecdotal evidence emerged that some patients did not feel well on LT4 and preferred to return to DTE.32,33
Continue to: Several clinical trials...






