Strategies for improved management of hypothyroidism
Management is clear-cut—yet many patients don’t reach treatment goals. To optimize quality of life, master the fine points of T4 replacement and address the impact of comorbidities.
PRACTICE RECOMMENDATIONS
› Prescribe levothyroxine (LT4) to maintain thyroid-stimulating hormone (TSH) at 4 to 7 mIU/L in select patients with primary hypothyroidism for whom that range of the serum TSH level can be considered appropriate (ie, those older than 65 years and those who have underlying coronary artery disease or another debilitating chronic disorder). A
› Counsel all women of childbearing age with primary hypothyroidism that they need to have their dosage of LT4 increased as soon as pregnancy is suspected. A
› Keep in mind that treating hypothyroidism is not always necessary in older patients who have subclinical disease and a serum TSH level < 10 mIU/L. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
These measurements must be interpreted within the context of the laboratory-specific normal range for each test. Third-generation serum TSH assays are more sensitive and specific than serum FT4 measurements for hypothyroidism. FT4 is usually measured by automated analogue immunoassay, which generally provides reliable results; abnormal binding proteins or other interferences occur in some patients, however, resulting in reporting of a falsely high, or falsely low, FT4 level. In such cases, FT4 by direct dialysis, or total T4, can be measured for further evaluation. In primary care, you are most likely to encounter primary hypothyroidism; secondary (central) hypothyroidism is much rarer (< 5% of cases).4
The ins and outs of treatment
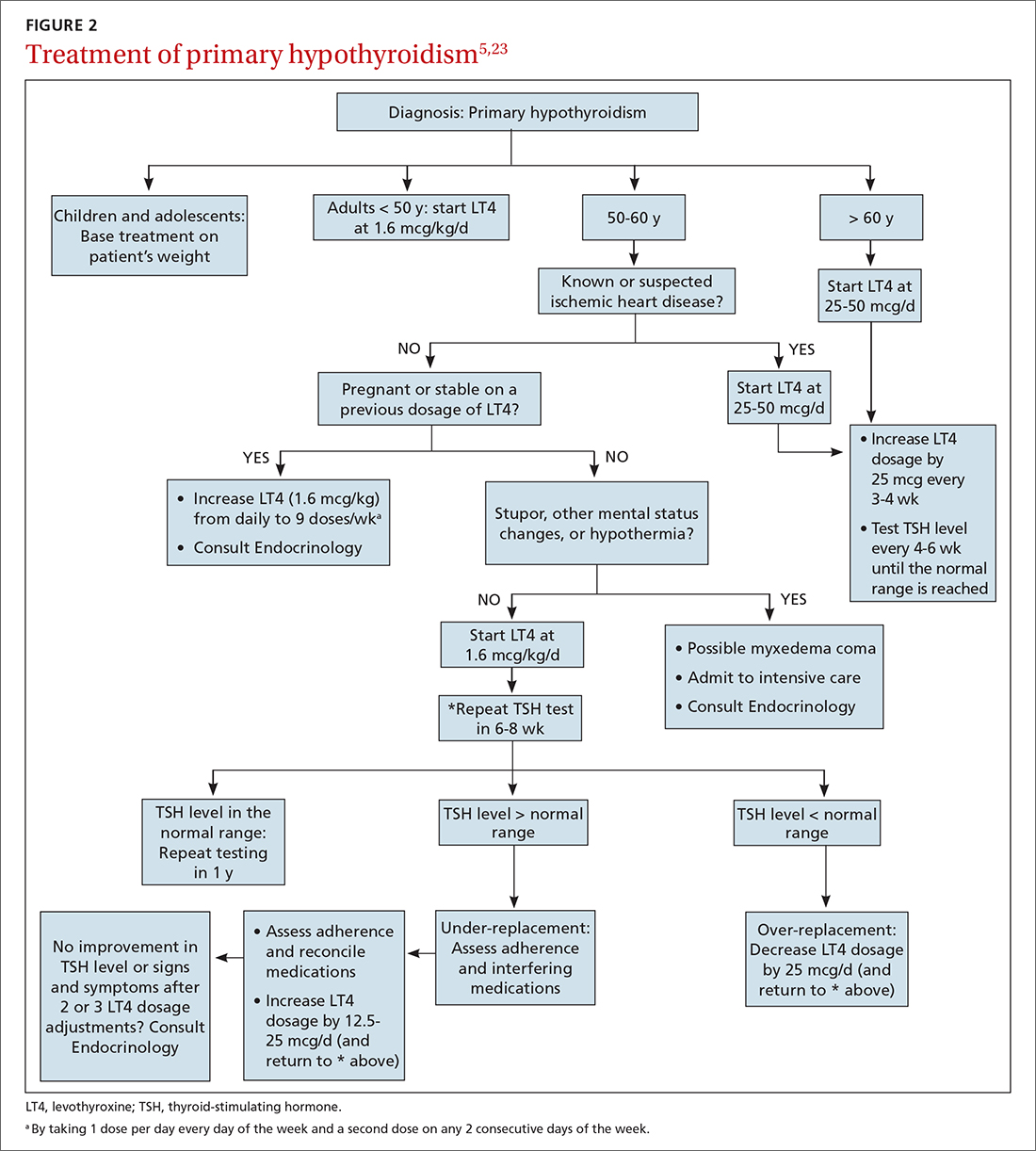
For most patients, hypothyroidism is a permanent disorder requiring lifelong thyroid hormone replacement therapy—unless the disease is transient (ie, painless or subacute thyroiditis); reversible, because it is caused by medication; or responsive to medical intervention that addresses the underlying autoimmune condition.19 Goals of treatment (Figure 25,23) are to:
- normalize the TSH level to 0.5-5.0 mIU/L (the main goal), with an age-related shift toward a higher TSH goal in older patients (and an upper limit of normal of 7.5 mIU/L in patients who are ≥ 80 years of age)20
- restore the euthyroid state
- relieve symptoms
- reduce any goiter
- avoid overtreatment (iatrogenic thyrotoxicosis).
Desiccated thyroid extract (DTE), developed in the late 1880s and made from the dried thyroid gland of pigs, sheep, or cows, was the earliest treatment for hypothyroidism. The use of DTE has declined since the introduction of synthetic thyroxine (T4, or levothyroxine [here, referred to as LT4]), which is now the standard treatment.20-22 LT4 is deiodinated in peripheral tissues to form T3, the active thyroid hormone; this process accounts for 80% of total T3 production daily.24
LT4 formulations. LT4 is commercially available in tablet, soft-gel, and liquid preparations. Most patients are treated with the tablet; the soft-gel capsule or liquid is an option for patients who absorb the tablet poorly (because of atrophic gastritis, celiac disease, or gluten sensitivity or because they are post bariatric surgery). Increasing the dosage of the tablet form of LT4, with ongoing TSH monitoring, is more cost effective than moving to an alternative preparation.
If a switch of LT4 formulation is made (ie, from one manufacturer to another), test the serum TSH level to ensure that the therapeutic goal is being reached. Also, in our experience, it is best to prescribe a brand-name preparation of levothyroxine, not a generic, whenever possible, due to the variability in generic formulations and the potential presence of other (inert) ingredients.25
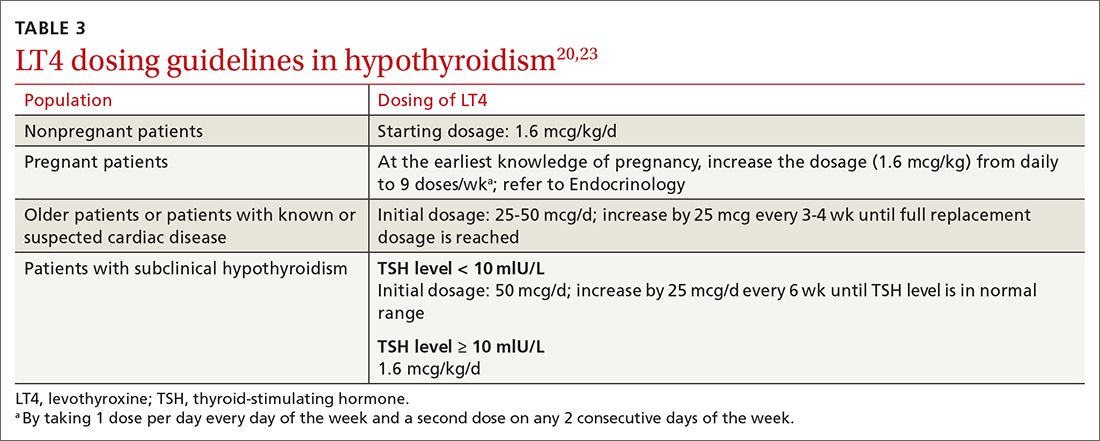
Dosing (TABLE 320,23). The average full replacement dosage of LT4 for a young, healthy adult is approximately 1.6 mcg/kg/d. Older patients (> 65 years) or those with coronary artery disease (CAD) should be started on a lower dosage (25-50 mcg/d) and titrated to goal accordingly.
LT4 (tablets, soft-gel capsules, or liquid) should be administered on an empty stomach, with water only, 30 to 60 minutes before breakfast. Medications that interfere with LT4 absorption (eg, bile acid resins, calcium carbonate, ferrous sulfate) should be taken several hours after LT4. For patients who cannot take LT4 in the morning, taking it at bedtime (≥ 2-3 hours after the last meal) is acceptable.
Continue to: Monitoring and titrating






