Scabies: Refine your exam, avoid these diagnostic pitfalls
Nearly half of all infections are missed when first examined. Attentiveness to specific details, particularly in 3 common scenarios, can help ensure an accurate Dx.
VIDEO shows scabies mite in motion
PRACTICE RECOMMENDATIONS
› Consider scabies with any severe pruritic eruption. Conduct a thorough physical exam, preferably with a dermatoscope, for burrows in the webs and sides of fingers, proximal palm, and wrists. A
› Consider scabies in all patients—especially the immunocompromised—who have distal white or yellow thick, scaly, or crusted plaques. C
› Include scabies in the differential when patients present with smooth nodules of the genitals or pruritic smooth papules and plaques in other locations. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
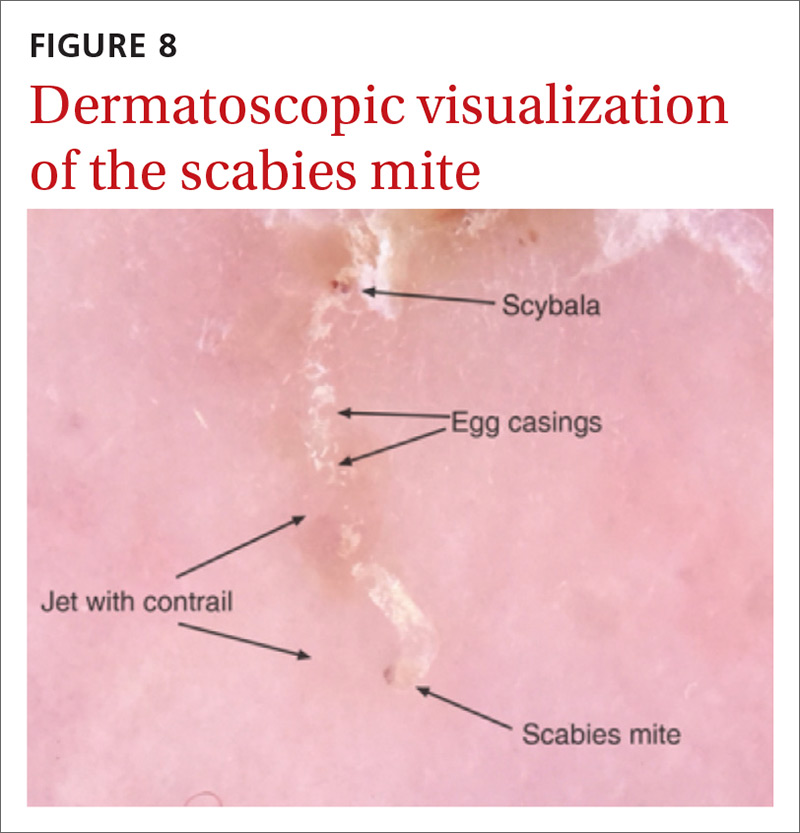
Handheld illumination with a dermatoscope will allow visualization of the mite (FIGURE 8). (See “How fast do scabies mites move? Dermoscopy video answers that question.”) Dermatoscope findings consistent with scabies include a “delta glider,” a dark triangular shape that is the mite’s head hidden in the burrow,20 or the classic “jet with contrail” (FIGURE 8).21 Scrape the burrow to discover the mature scabies mite (FIGURE 9) and confirm the diagnosis.
Microscopic examination of scrapings has a reported sensitivity and specificity of up to 90% and 100%, respectively, when collection of scrapings is performed accurately and contains ova, feces, or mites.14,20,22 Dermatologists increasingly use dermatoscopes to diagnose scabies. Dermoscopy's sensitivity is 91% and specificity is 85% to 86%,14 which is a reassuring frame of reference for physicians who do not routinely use dermatoscopes and instead rely on scrapings.

Continue to: How fast do scabies mites move? Dermoscopy video answers that question






