Scabies: Refine your exam, avoid these diagnostic pitfalls
Nearly half of all infections are missed when first examined. Attentiveness to specific details, particularly in 3 common scenarios, can help ensure an accurate Dx.
VIDEO shows scabies mite in motion
PRACTICE RECOMMENDATIONS
› Consider scabies with any severe pruritic eruption. Conduct a thorough physical exam, preferably with a dermatoscope, for burrows in the webs and sides of fingers, proximal palm, and wrists. A
› Consider scabies in all patients—especially the immunocompromised—who have distal white or yellow thick, scaly, or crusted plaques. C
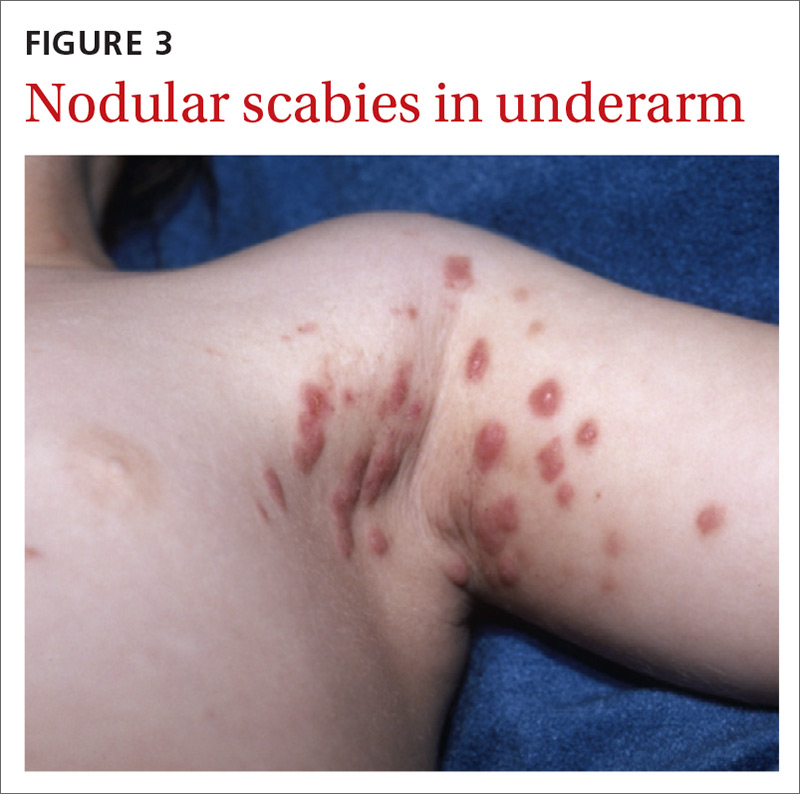
› Include scabies in the differential when patients present with smooth nodules of the genitals or pruritic smooth papules and plaques in other locations. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Nodular scabies variants can masquerade as pseudolymphoma, lymphoma, or leukemia cutis. In immunocompromised and elderly individuals, crusted scabies is often mistaken for psoriasis, atopic dermatitis, keratoderma, and lichen planus.2,4,5
Scabies’ classic presentation
Typically, scabies causes intensely pruritic erythematous papules. Areas commonly affected are the webs and sides of fingers (FIGURE 1A and 1B), proximal palm and wrist flexors, extensor aspects of the arms and legs, axillary folds, periumbilical areas, the peri-areolar region in women, buttocks and thigh creases, and, in males, the genitals. The head may also be affected in children (FIGURE 1C), but seldom in adults. Interestingly, the back is usually spared across all age groups, though not always (FIGURE 2).
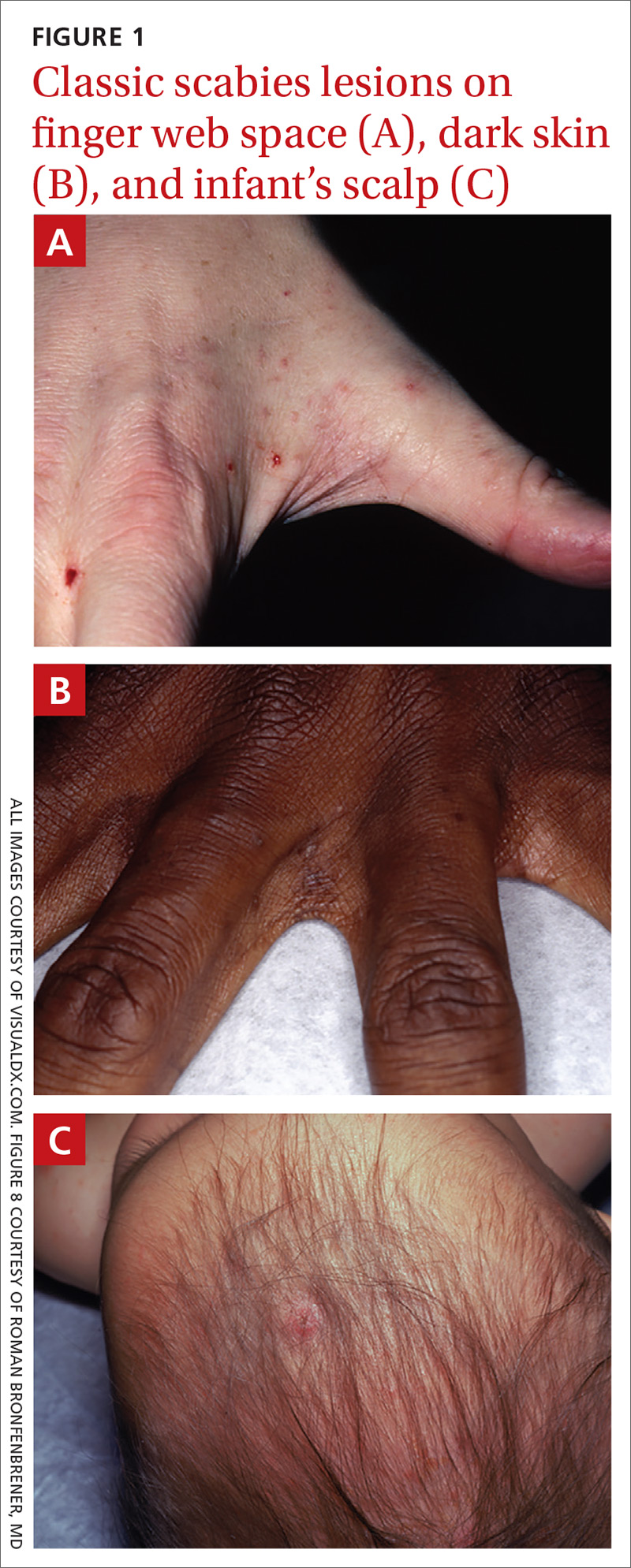

The classic presentation also varies across age groups and populations.2 In children, vesicles, pustules, and nodular pruritic lesions may coexist with eczema and impetigo. Among homeless individuals, coinfection with impetigo and eczema is common.
Scabies subtypes with varying presentations
Clinical manifestations of scabies subtypes may make it difficult to diagnose the disease. These subtypes include nodular, pustular, vesiculobullous, and crusted scabies (Norwegian scabies). Although rare, these subtypes merit acknowledgement, as atypical cases contribute to the high rate of misdiagnosis.
Nodular scabies is a clinical variant that accounts for about 7% of scabies cases.7 It can resist traditional scabies treatment (permethrin cream, ivermectin—which we’ll discuss in a bit) and often requires topical or intralesional corticosteroid management. Nodular scabies most commonly affects male genitalia. Patients may have multiple excoriated skin-colored erythematous papules and nodules in areas involving the classic distribution of scabies (web spaces of fingers, flexural areas [FIGURE 3], scrotum, and groin).8
Continue to: Pustular scabies...






