Psychosis in women: Consider midlife medical and psychological triggers
Estrogen loss, other factors increase vulnerability for women after age 40
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
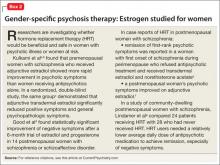
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others