The puzzling self-poisoner
Ms. M tried to kill herself with rat poison, and her coagulation values continue to rise. Is she secretly consuming more poison in her hospital room?
I was skeptical that escitalopram could be contributing to Ms. M’s rising anticoagulation values. Selective serotonin reuptake inhibitors have antiplatelet effects, but platelet function does not affect INR to the degree we were observing.
‘Superwarfarins’
Physicians had advised us that Ms. M’s INR should decrease under the assumption that rat poison is for all practical purposes the same as warfarin, but we had not investigated distinctions between the 2 compounds. A literature search revealed that several rat poisons are not simply warfarin repackaged as a pesticide. Most are “superwarfarins”—chemicals similar to warfarin but more potent and with a much longer half-life.2 Case report data suggest the plasma half-life of these chemicals is 20 to 62 days.3
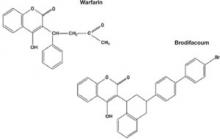
Most commercial rat poisons are made of brodifacoum, which has a chemical structure similar to warfarin but with an additional long polycyclic hydrocarbon side chain (Figure 1). The potency of brodifacoum compared with warfarin is approximately 100 to 1.4-6 The chemical is highly lipophilic and can stay in the body for an extended period.4-6 Lab tests can measure serum brodifacoum levels.3
After Ms. M identifies the brand name of the rat poison she ingested, we contact the American Association of Poison Control Centers and verify the agent she used was brodifacoum. This explains why her INR was not decreasing—but does not explain the increase.
A drug interaction? Because Ms. M’s liver function is within normal limits, the next theory to investigate is if brodifacoum is interacting with any medications she is taking. I could not find any medical journal articles, programs, or Web sites describing brodifacoum’s interactions with medications. After all, brodifacoum is a pesticide, not a medication.
I considered that because brodifacoum and warfarin have a similar structure and function, they may interact with medications in a similar manner. After another literature search, only acetaminophen had evidence of interaction with warfarin that could explain her rising INR.
Documentation of interactions between warfarin and acetaminophen are sparse. In one case, a 74-year-old man receiving warfarin for atrial fibrillation experienced an abrupt increase in INR after taking acetaminophen.7 In a double-blind, placebo controlled, randomized trial of patients taking warfarin, INR rose rapidly after the start of acetaminophen and was significantly increased within 1 week compared with patients receiving placebo.8
Figure 1 Chemical structures of warfarin and rat poison
Most commercial rat poisons are made of brodifacoum, which is chemically similar to warfarin but has an additional long polycyclic hydrocarbon side chain.
FOLLOW-UP: Analgesic substitution
We suggest to the physician that Ms. M’s INR may be increasing because of an interaction between brodifacoum and acetaminophen, which she took several times a day. On day 8 of Ms. M’s hospitalization, the physician discontinues acetaminophen and prescribes ibuprofen, 400 mg tid as needed for pain, and pantoprazole, 40 mg/d, to prevent GI bleeding from possible irritation caused by ibuprofen. The team continues to monitor Ms. M’s coagulation values.
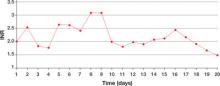
Within a day of discontinuing acetaminophen, Ms. M’s INR decreased as expected (Figure 2). The rest of her medication regimen is continued, and her INR levels continued to decrease.
One-to-one observation is discontinued. However, because of the patient’s continued determination to end her life and no significant improvement in her depression, Ms. M is considered a danger to herself and involuntary inpatient hospitalization is continued.
Figure 2 Ms. M’s INR values during hospitalization
The patient’s INR values began to rise mysteriously after she was transferred to the inpatient psychiatric unit. Acetaminophen was discontinued on day 8, and within a day her INR values began to drop.
INR: International normalized ratio
The author’s observations
Poisoning is a common method of attempting suicide, patients may use substances that clinicians rarely encounter. For most toxic, nonmedication substances, data on interactions with medications are sparse. if you suspect your patient has ingested a toxic substance with which the treatment team has little experience, contact the American Association of Poison Control Centers at 800-222-1222.
Suspect superwarfarin poisoning in suicidal patients with coagulopathy, prolonged prothrombin time, and elevated INR that does not respond to large amounts of vitamin K.9,10 These patients are at high risk of successfully completing suicide because of superwarfarins’ long half-life and daily maintenance required to keep coagulation levels within a safe range for at least several weeks.
The most serious complication these patients face is intracranial hemorrhage, which occurs in 2% of patients with excessive warfarin-based coagulation and is associated with a 77% mortality rate.11 GI bleeding occurs in 67% of these patients.2