Avoiding EPS is key to realizing ‘atypical’ benefits
CATIE finding is not unique to one antipsychotic class.
CATIE found no difference among the various FGAs and SGAs with regard to overall efficacy, effects on cognition, and occurrence of tardive dyskinesia in treating chronic schizophrenia. Perhaps it was CATIE’s failure to find a difference in EPS that explains its inability to demonstrate FGA-SGA differences in cognition and other effectiveness domains.
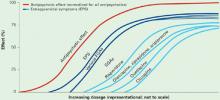
Figure Dose-response curves: Antipsychotic vs extrapyramidal effects
All FGAs and SGAs produce an equivalent antipsychotic effect (red), but they vary in the degree of separation between dosages at which their antipsychotic and extrapyramidal effects occur.
Source: Adapted from reference 13
What catie tells us
The exaggerated view of SGAs as uniformly more efficacious, safer, and better tolerated than FGAs needs to be revised. At the same time, however, the results of CATIE should not be over-interpreted. They tell us that if the four phase 1 SGAs and the FGA perphenazine are used at certain dosages in a particular manner in a specific schizophrenia population—chronic, moderately ill, without tardive dyskinesia—then no differences might be expected among these antipsychotics. But CATIE’s findings might not generalize beyond individuals with schizophrenia at low risk for EPS.
CATIE underlines the importance of achieving an adequate antipsychotic effect without EPS and without using anticholinergics. Clinical consequences of EPS extend beyond motor manifestations and include:
- worse cognition (bradyphrenia)
- worse negative symptoms (neuroleptic-induced deficit syndrome)
- worse depression and suicidality (neuroleptic dysphoria)
- higher risk of tardive dyskinesia.20
SGAs’ presumed ability to provide broader efficacy—cognition, negative symptoms, dysphoria—and lower risk of tardive dyskinesia appears to be driven by their lower EPS liability in association with an equivalent antipsychotic effect. Evidence for an SGA advantage independent of this effect is weak.21,22
Thus, CATIE’s inability to find an FGA-SGA difference in EPS might explain its failure to observe an FGA-SGA difference in cognition and other effectiveness domains.
The clinical pearl
Avoiding EPS and anticholinergics appears to be the key to improving cognition, dysphoria, and negative symptoms with FGAs and SGAs. SGAs’ ability to achieve an equivalent antipsychotic effect without EPS also seems related to their lower risk of tardive dyskinesia.
SGAs’ main advantage may be their greater ease of achieving an adequate antipsychotic effect without EPS or the need to add an anticholinergic to treat or prevent EPS. This comes from the broader separation between dosages at which SGAs produce their antipsychotic versus EPS effects, compared with FGAs (Figure).13
In clinical practice, then, we must achieve an adequate antipsychotic effect for our patients without EPS—whether we are using FGAs or SGAs—to obtain “atypical” benefits. The purported benefits of an “atypical” antipsychotic are not unique to a particular class of agents but relate to achieving a good antipsychotic effect without EPS—and the SGAs are better able to accomplish this than the FGAs.
Careful EPS monitoring is crucial to achieving optimal antipsychotic therapy. Reduced emphasis on EPS in the past decade (in awareness of EPS and training to detect symptoms) and overlap between behavioral aspects of EPS and psychopathology need to be addressed.
CATIE confirms clinical observations that:
Different agents are associated with different adverse effects, which can make achieving maximum efficacy and safety/tolerability challenging.
But differences among antipsychotics and heterogeneity in individual response and vulnerabilities may allow us to optimize treatment.
Different agents at different dosages may provide the best outcomes for individual patients, and the optimal agent and/or dosage can vary in the same patient at different stages of the illness. The CATIE trial contributes to evidence that guides our efforts to provide optimal antipsychotic treatment of schizophrenia (Table 3). Its “surprising” findings are most useful when considered in the context of the database to which it adds.25
Table 3
Treating chronic schizophrenia: 4 clinical tips from CATIE
| Minimizing extrapyramidal symptoms (EPS) is essential, whether using FGAs or SGAs |
| Avoiding EPS and not using adjunctive anticholinergics is the key to SGAs’ purported benefits, such better cognition, less dysphoria, lower negative symptom burden, and lower risk of tardive dyskinesia |
| Antipsychotic dosing is key to accomplishing an adequate antipsychotic effect without EPS |
| Match the antipsychotic choice and dosage to the individual patient’s vulnerability, then make adjustments based on response |
Related resources
- Tandon R. Comparative effectiveness of antipsychotics in the treatment of schizophrenia: What does CATIE tell us? Parts 1 and 2. Int Drug Ther Newsl 2006;41:51-8;67-74.
- Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia study. www.catie.unc.edu/schizophrenia.
Drug brand names
- Clozapine • Clozaril
- Fluphenazine • Permitil
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.