INTERSTITIAL CYSTITIS: The gynecologist’s guide to diagnosis
Don’t overlook this disease when a patient complains of pelvic pain. As many as 85% of women who seek care for chronic pelvic pain have interstitial cystitis and painful bladder syndrome, studies show—instead of, or in addition to, a gynecologic diagnosis.
IN THIS ARTICLE
Despite controversy over nomenclature and diagnostic criteria, there is no uncertainty that the lives of women who have IC/PBS are significantly altered by the disease. It adversely affects leisure activity, family relationships, and travel in 70% to 94% of patients.3 Suicidal thoughts are three to four times more likely in women who have IC/PBS than in the general population. Quality of life is markedly decreased across all domains, and depressive symptoms are much more common in women who have IC/PBS than in the general population.4
IC/PBS appears to affect women more often than men, and it is a frequent diagnosis among women who have chronic pelvic pain. For example, in a primary care population of women 15 to 73 years old who had chronic pelvic pain, about 30% were determined to have pain of urologic origin.5 It has been suggested, based on symptoms of urgency-frequency and a positive potassium sensitivity test, that approximately 85% of women who see a gynecologist for chronic pelvic pain have IC/PBS in addition to or instead of a gynecologic diagnosis.6 Among women given a diagnosis of endometriosis, 35% to 90% have been found to have IC/PBS as well.

FIGURE 1 Glomerulations are a common finding
Cystoscopy with hydrodistention often, but not always, reveals glomerulations (mucosal hemorrhages) in a patient who has interstitial cystitis.
Two screening tools may aid the diagnosis
IC/PBS is a clinical diagnosis, based on symptoms and signs. Although some controversy surrounds this statement, there is no question that we lack a gold-standard test to reliably make the diagnosis.
Two screening instruments are commonly used to identify patients in whom IC/PBS should be considered. One is the O’Leary-Sant questionnaire (TABLE 1), which incorporates two scales:
- the IC Symptom Index (ICSI)
- the IC Problem Index (ICPI).
The O’Leary-Sant questionnaire was not designed specifically to diagnose IC/PBS but to aid in its evaluation and management and to facilitate clinical research.
TABLE 1 The O’Leary Sant IC questionnaire
Please mark the answer that best describes your bladder function and symptoms.
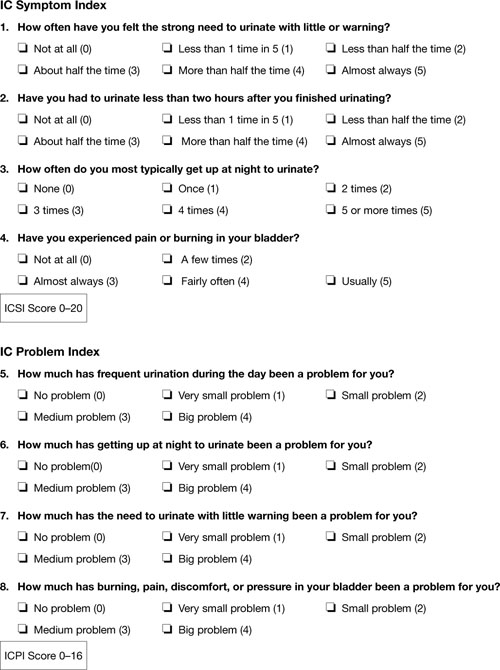
TABLE 2
The Pelvic Pain and Urgency/Frequency Symptom Scale
Please circle the answer that best describes your bladder function and symptoms.
| 0 | 1 | 2 | 3 | 4 | ||
| 1. | How many times do you go to the bathroom DURING THE DAY (to void or empty your bladder)? | 3-6 | 7-10 | 11-14 | 15-19 | 20 or more |
| 2. | How many times do you go to the bathroom AT NIGHT (to void or empty your bladder)? | 0 | 1 | 2 | 3 | 4 or more |
| 3. | If you get up at night to void or empty your bladder, does it bother you? | Never | Mildly | Moderately | Severely | |
| 4. | Are you sexually active? No ___ Yes ___ | |||||
| 5. | If you are sexually active, do you now or have you ever had pain or symptoms during or after sexual intercourse? | Never | Occasionally | Usually | Always | |
| 6. | If you have pain with intercourse, does it make you avoid sexual intercourse? | Never | Occasionally | Usually | Always | |
| 7. | Do you have pain associated with your bladder or in your pelvis (lower abdomen, labia, vagina, urethra, perineum)? | Never | Occasionally | Usually | Always | |
| 8. | Do you have urgency after voiding? | Never | Occasionally | Usually | Always | |
| 9. | If you have pain, is it usually | Mild | Moderate | Severe | ||
| 10. | Does your pain bother you? | Never | Occasionally | Usually | Always | |
| 11. | If you have urgency, is it usually | Mild | Moderate | Severe | ||
| 12. | Does your urgency bother you? | Never | Occasionally | Usually | Always | |
| PUR Score 0–35 | ||||||
In a busy gynecologic practice, routine use of one of these questionnaires can greatly facilitate identification of patients who may have IC/PBS.
Diagnosis can be straightforward—but often it isn’t
In many patients, diagnosis of IC/PBS is straightforward, with classic findings:
- pelvic pain
- urinary frequency (voiding every 1 or 2 hours)
- discomfort or increased pain (as opposed to a fear of losing urine) leading to urinary urge
- significant tenderness during single-digit palpation of the bladder at the time of pelvic examination
- nocturia in many cases.
Be aware that diagnosis can be more challenging when the patient is in the early course of the disease. About 90% of patients who have IC/PBS have only one symptom in the beginning—fewer than 10% experience the simultaneous onset of urgency, frequency, nocturia, and pain. The mean time from development of the initial symptom until manifestation of all symptoms ranges from 2 to 5 years.7 In about one third of patients, the initial symptom is urinary frequency and urgency preceding the onset of pain—but almost equal numbers of patients develop pelvic pain as a solitary symptom before the onset of any urinary symptoms.
Complicating matters is the fact that symptoms are often episodic early in the course of the disease. The episodic nature of symptoms often leads to multiple misdiagnoses such as urinary tract infection and recurrent or chronic cystitis. A history of empiric treatment of recurrent urinary tract infection without documentation of a positive culture is common in women who have IC/PBS. A patient who has early interstitial cystitis may respond to antibiotic treatment due to the natural waxing and waning of symptoms, the placebo effect, or an increase in fluid intake that usually accompanies antibiotic usage (dilute urine is less irritating to the bladder). Awareness of the possibility of IC/PBS in these patients is essential if diagnosis is to be made as early as possible.






