UPDATE: MENOPAUSE
We’re learning more about the long-term risks and benefits of hormone therapy, how to assess and treat osteoporosis, and the need for vitamin D
IN THIS ARTICLE
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. https://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
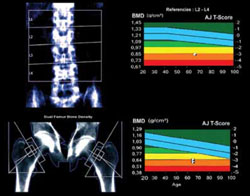
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).







