Management of prolonged decelerations
Some are benign, some are pathologic but reversible, and others are the most feared complications in obstetrics
Avoid fetal pulse oximetry
Although fetal pulse oximetry is FDA-approved and commercially available in the United States, and may be well suited for monitoring fetal arrhythmias,19,20 a prolonged deceleration is an absolute contraindication to its use.21
Summary
Overall, in managing a delivery marked by prolonged decelerations, we should strive to minimize maternal–fetal complications by carefully assessing the clinical situation, correcting reversible problems, and preparing for expeditious delivery if the fetal condition is of sufficient concern that further expectant management is unlikely to allow for safe spontaneous delivery. Still, “…bedside judgment inevitably will sometimes be imperfect given the unpredictability of these decelerations.”2
The author reports no financial affiliations relevant to this article.
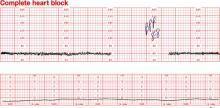
Dilemma: Fetal bradycardia due to congenital complete heart block secondary to anti-SSA/Ro and anti-SS-B/La antibodies. The fetal ventricular rate is fixed at 60 bpm
Management: At 30 weeks’ gestation, with no sonographic evidence of heart failure and a biophysical profile score of 8/8, expectant management is indicated
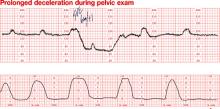
Dilemma: Prolonged deceleration during pelvic examination in an uncomplicated term pregnancy. Note that fetal heart rate (FHR) variability was maintained during recovery of the FHR baseline
Outcome: Uneventful spontaneous vaginal delivery
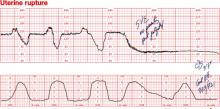
Dilemma: Prolonged deceleration due to uterine rupture during trial of labor after cesarean. Repetitive variable decelerations preceded the prolonged deceleration. FHR variability was lost after several minutes
Management: Emergency cesarean