Interstim: An implantable device for implacable urinary symptoms
Urge incontinence, urgency–frequency, and retention may yield to electrical stimulation
IN THIS ARTICLE
At 6 months, stimulation was turned off in 23 of the 26 patients in the treatment group. (One had the InterStim system explanted, and 2 refused to have the device turned off due to fear of return of symptoms.) When stimulation was turned off, symptoms did return to baseline. At 12 months, when the stimulation was turned back on, patients regained improvement in their urinary indices, which remained statistically significant. At 24 months, only 21 patients were evaluated on all analyses. The researchers reported that 43% of patients had maintained either fewer than 7 voids per day or at least a 50% reduction in the number of daily voids.
Although this report looked at effectiveness in only 51 patients, it did utilize a randomization method. A larger cohort, of 196 patients, was studied in a retrospective and prospective trial conducted by Spinelli and colleagues.
SHORT- AND LONG-TERM EFFICACY
Spinelli M, Bertapelle F, Cappellano F, et al, on behalf of the GINS Group. Chronic sacral neuromodulation in patients with lower urinary tract symptoms: results from a national register. J Urol. 2001;166:541–545.
A national register was created in Italy to collect results from all centers that were performing sacral neuromodulation. The investigators analyzed a total of 196 patients (46 males and 150 females).
Retrospective analysis
A total of 93 (18 male and 75 female) of the 196 were included, and 61 of the 93 patients were available for assessment. Mean follow-up was 41 months.
Prospective analysis
A total of 103 patients (28 males and 75 females) were followed, using voiding diaries, number of incontinence episodes, residual urine volume, number of catheterizations, pad use, and pain symptoms. Assessments were performed before percutaneous nerve evaluation and at 3-month intervals for 1 year, and at 6-month intervals for up to 2 years.
Detrusor instability. In the prospective register, 42 patients had detrusor instability. Compared with baseline, the mean number of incontinence episodes declined from 5.4 to1.1 at 12 months; 75% of patients had fewer than 8 micturitions per day at 3 months and 84% had fewer than 8 micturitions per day at 6 months, and this rate remained stable at 12 and 18 months. At 3 months, 57% of the study population was dry; at 6 months, 65% compared with baseline. At 18 months, 43% of the patients were completely dry. Improved quality of life was found in the patients with detrusor instability.
Voiding disorders. Of 103 patients, 35 had voiding disorders. At 3 and 6 months, 67% had stopped catheterization and 13% were catheterizing only once per day. At 9 and 12 months, 50% were not catheterizing and 33% to 13% were catheterizing once per day; 67% were not catheterizing at 18 months. However, the remaining 33% of patients had fluctuating results.
Complications and adverse events. In patients followed prospectively, 15.5% required surgical revision of the InterStim system due to pain at the implantation or to cable connection site or wound problems such as hematoma or lead fracture. Complete removal was performed in 3.9%.
ADDITIONAL REFERENCES
- Leng WW, Chancellor MB. How sacral nerve stimulation neuromodulation works. Urol Clin N Am. 2005;32:11–18.
- Weil EHJ, Ruiz-Cerda JL, Eerdsmans PHA, et al. Sacral root neuromodulation in the treatment of refractory urinary urge incontinence: a prospective randomized clinical trial. Eur Urol. 2000;37:161–171.
Sacral neuromodulation stimulation (SNS) is a minimally invasive treatment for refractory urinary urge incontinence, urinary urgency–frequency alone or in combination, and urinary retention
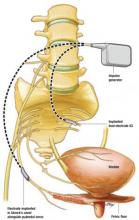
The InterStim implantable system comprises a lead with 4 electrodes and an extension cable. Its programmable impulse generator, usually placed in the upper buttock region, sends mild electrical pulses to the sacral nerve
Stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying
Stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter. Contraction and relaxation of these muscles are integral to micturition and bladder storage
2 guarding reflexes prevent incontinence: 1) between the bladder and the smooth muscles of the urethra, which is mediated by the efferent pathways of the sympathetic system, and2) between the afferent nerves in the bladder and the efferent pathways in the pudendal nerve, leading to contraction of the skeletal component of the urethra
Bladder afferent pathways are mediated by unmyelinated C fibers that detect noxious stimuli and trigger voiding, and by small myelinated A fibers that detect bladder muscle tension or fullness
Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and turn off overactive voiding by blocking ascending sensory pathways