Reducing the legal risks of labor induction and augmentation
Specific tactics minimize the chance of adverse oxytocin-related outcomes—and a flurry of allegations
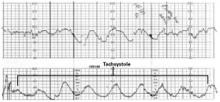
Decrease or discontinue oxytocin when variant fetal heart rate patterns suggest decreased uteroplacental perfusion. This tracing shows uterine hyperstimulation (tachysystole with decelerations).
FIGURE 2 Titrate oxytocin to “normalize” contractions
Consider decreasing oxytocin—or avoid further increases—when uterine contractions are more frequent than 5 in 10 minutes or 7 in 15 minutes. This tracing shows 6 uterine contractions in 10 minutes. The fetal heart rate channel demonstrates moderate variability and, therefore, fetal tolerance of a frequent contraction pattern.
Why policies and procedures are a double-edged sword
Although policies and procedures are intended to help guide health care assessments and interventions, they are routinely subpoenaed and entered as evidence in an attempt to define the standard of care. Failure to follow these policies and procedures may be viewed by expert witnesses as a breach in that standard.
Use of oxytocin requires a medical or nursing professional to make judgments based on training, experience, and knowledge. Although policies and procedures cannot address every possible scenario or replace informed judgment, physicians and nurses are routinely criticized for failing to administer oxytocin or otherwise proceed exactly as outlined.
Some reasons policies and procedures should not be viewed as standard of care:
- They are typically written by a person in an administrative position who does not actually provide the care outlined.
- They are usually not routinely updated as new literature is published.
- Since they do not provide guidelines for unanticipated or unusual situations, deviation from policy is reasonable and even necessary in many scenarios.
- They are rarely written to reflect “reasonable” care; instead, they suggest an “ideal” level of care.
Reasonable protocols. Every physician and health care provider should be familiar with the hospital’s policies and procedures and help hospital personnel revise those that appear to limit the physician’s ability to easily adjust care or exercise judgment. Among the suggestions:
- Make all recommendations practical. This means they can be followed most of the time in most situations.
- Avoid terms such as “mandatory,” “always,” “never,” “should,” or “must.”
- Limit recommendations that can be considered “endpoints” for increasing oxytocin, such as: “Increase oxytocin until contractions are 2 to 3 minutes apart and 60 seconds in duration.” Recommendations written in this fashion are difficult to follow clinically; although the criteria may be met, labor may not progress, warranting an increase in oxytocin beyond the endpoints in the guidelines. Guidelines that discuss considerations for decreasing or discontinuing the drug would be better.
It also is important to foster understanding among medical and nursing staff that policies and procedures are guidelines and that medical and nursing judgment supersedes policy recommendations.
The authors report no financial relationships relevant to this article.