Ectopic pregnancy: A 5-step plan for medical management
Two experts describe a multidose methotrexate regimen, the first choice for unruptured, uncomplicated ectopics.
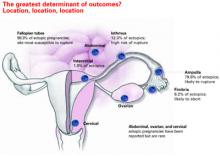
How size influences management
Ultrasound can detect ectopic pregnancies as small as 2 cm. In general, an ectopic sac size larger than 4 cm should be treated surgically.
STEP 4Perform uterine curettage
If ultrasound imaging is inconclusive and ß-hCG levels are plateauing or rising subnormally, perform uterine curettage. If ß-hCG levels decrease 15% or more 8 to 12 hours after the procedure, a complete abortion can be strongly suspected.21 If ß-hCG levels plateau or rise, the trophoblasts were not removed by curettage, and ectopic pregnancy is diagnosed.21
Keep in mind these important points:
- Without uterine curettage, roughly 40% of ectopic pregnancy diagnoses are incorrect.22
- Because curettage will result in termination of pregnancy, it is vital that it be limited to cases involving abnormal ß-hCG levels, not normally rising values.
STEP 5Administer methotrexate
Medical management is indicated when the following circumstances are present:
- No viable intrauterine pregnancy is present.
- No rupture has occurred.
- Any adnexal mass is 4 cm in size or smaller.
- ß-hCG levels are below 10,000 mIU/mL.
If there is a positive fetal heart beat, surgery is preferred.
Firm diagnosis of ectopic pregnancy is essential prior to methotrexate administration. If the drug is given to a woman carrying a viable pregnancy, it may result in loss of the pregnancy or methotrexate embryopathy.23
How methotrexate resolves ectopic pregnancy
Systemic methotrexate has been used successfully in the treatment of ectopic pregnancy for more than 20 years. A folic acid antagonist, it inhibits de novo synthesis of purines and pyrimidines. It thus interferes with DNA synthesis and cell multiplication.24 Actively proliferating trophoblasts are particularly vulnerable.25
When methotrexate is administered to normally pregnant women, it blunts the normal ß-hCG increment over the next 7 days. Circulating progesterone and 17-a-hydroxyprogesterone concentrations also decline, and abortion occurs.26
Methotrexate directly impairs trophoblastic production of hCG; the decrement in corpus luteum progesterone is a secondary event.
Side effects include abdominal distress, chills and fever, dizziness, immunosuppression, leukopenia, malaise, nausea, ulcerative stomatitis, photosensitivity, and undue fatigue.
Breastfeeding is an absolute contraindication to methotrexate, while relative contraindications include abnormal liver function tests, blood dyscrasias, excessive alcohol consumption, HIV/AIDS, psoriasis, ongoing radiotherapy, rheumatoid arthritis, and significant pulmonary disease.
Multiple-dose methotrexate is superior
In a recent meta-analysis comparing single-and multiple-dose regimens of methotrexate, Barnhart and colleagues4 found the latter to be more effective, although the single dose was more commonly given. The single-dose regimen was associated with a significantly greater chance of failure in both crude (OR 1.71; 1.04, 2.82) and adjusted (OR 4.74; 1.77, 12.62) analyses. Consequently, we advocate the multiple-dose regimen detailed in TABLE 2: 1 mg of methotrexate per kilogram of body weight on day 1, alternating with 0.1 mg of leucovorin per kilogram on succeeding days. Continue this regimen until ß-hCG levels decline in 2 consecutive daily titers, or 4 doses of methotrexate are given, whichever comes first.
If treatment is unsuccessful after 4 doses, additional methotrexate is unlikely to be effective and will involve significant additional cost and morbidity. If ß-hCG levels plateau or continue to rise, surgery is indicated.
Although multiple-dose therapy is more effective than a single dose, the optimal number of doses probably falls somewhere between 1 and 4.4 A 2-dose protocol currently under investigation may provide an optimal compromise.
Artificially high efficacy rates with “single-dose” therapy. Unusually high success rates in initial studies of the single-dose regimen may have been due to the inclusion of spontaneously aborting intrauterine pregnancies.27 Although 6 subsequent studies—1 cohort and 5 case-control studies involving 304 patients—found an overall success rate (no surgical intervention) of 87.2%, 11.5% of participants required more than 1 dose.9
Still the standard. Despite its lower efficacy rates, single-dose methotrexate remains the “standard” in the United States, as recommended in an American College of Obstetricians and Gynecologists practice bulletin.28 The usual intramuscular dose is 50 mg per square meter of body surface area, with ß-hCG titers on days 4 and 7 and an additional dose if ß-hCG levels fail to resolve.
What the evidence shows
Multidose methotrexate. Twelve studies measured the success of multiple-dose systemic methotrexate (TABLE 3); they included 1 randomized, controlled trial, 1 cohort study, and 10 case series. Between 1982 and 1997, 325 cases were treated with multiple-dose methotrexate. Of these, 93.8% had successful resolution with no subsequent therapy, and 78.9% of the 161 women tested had patent oviducts. In addition, of 95 women hoping to conceive, 57.9% had a subsequent intrauterine pregnancy and 7.4% developed a recurrent ectopic pregnancy. These rates compared favorably with numerous laparoscopic surgery series published during the same years.9