PPROM: New strategies for expectant management
Since antibiotics prolong latency in most cases, expectant management has become more feasible, with fewer morbidities at the time of delivery.
Gestational age determines management
The number 1 factor determining management is gestational age.
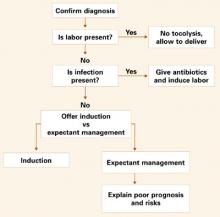
Before 23 weeks, the pregnancy is considered previable
Counsel these patients about the risk of infection, the prognosis of extreme prematurity, and the generally poor outcome of these pregnancies, which can involve pulmonary hypoplasia secondary to severe oligohydramnios (FIGURE 1).
Induction of labor is an option to terminate the pregnancy. If the patient chooses expectant management, monitor her closely for infection.4 Outpatient management is acceptable for the highly compliant patient. However, once fetal viability is attained, readmit the patient to monitor maternal and fetal well-being.
Between 23 and 32 weeks
Treat these women expectantly in the hospital unless there is evidence of infection or fetal compromise. Management includes intravenous antibiotic therapy and corticosteroids, as recommended by the National Institutes of Health (FIGURE 2).5
Although it is controversial, consider magnesium sulfate tocolytic therapy if the patient is actively contracting with no evidence of infection.6
Some authorities recommend amniocentesis (at any gestational age) to rule out infection prior to expectant management, while others consider the appropriate use of clinical parameters to be adequate.6
After monitoring the patient in the labor suite for 24 to 48 hours, transfer her to the antenatal ward, if she is stable, for frequent fetal surveillance and maternal evaluation. Continue to evaluate her for signs of intraamniotic infection such as fever, uterine tenderness, and foulsmelling discharge.
Many authorities recommend daily nonstress testing or biophysical profiles to evaluate fetal well-being.7
Between 32 and 34 weeks
Management for this gestational age range is the most controversial (FIGURE 3). Mercer et al8 demonstrated that expectant management is harmful to the neonate if fetal lung maturity is present. Most experts contend that some method of fetal lung assessment should be undertaken. The most effective method is sampling amniotic fluid by amniocentesis. Not only can fetal lung maturity be determined, but the fluid can be analyzed for evidence of infection using the Gram stain, glucose level, and white blood cell count.
When an amniocentesis site is unavailable, consider assessing fetal lung maturity via a pooled amniotic fluid sample from the vagina.9 Deliver the infant if either intraamniotic infection or fetal lung maturity is present.
If there is no evidence of fetal lung maturity, expectant management is usually recommended for pregnancies between 32 and 34 weeks.
In a recent survey of maternal-fetal medicine specialists in the United States, 58% recommended delivery at 34 weeks of gestation.10
For patients who are at less than 34 weeks upon presentation—or to be treated expectantly—consider giving antibiotics, corticosteroids, and tocolysis during the first 48 hours.
FIGURE 1 Managing premature rupture of membranes: Less than 23 weeks’ gestation
FIGURE 2 Managing premature rupture of membranes: 23 to <32 weeks’ gestation
The new standard of care: antibiotic therapy
In the 1980s, several studies suggested antibiotics were beneficial for PPROM patients.11 More recently, the Maternal-Fetal Medicine Network published the results of a large, prospective, randomized, double-blind, placebo-controlled trial clearly demonstrating that antibiotics prolong the latency period and decrease neonatal morbidities (see “Antibiotics in PPROM improve outcomes in Maternal-Fetal Medicine Network study”).12
Limited- versus broad-spectrum antibiotics
Although antibiotic therapy is now the standard of care for patients with PPROM, it remains unclear which antibiotic is best. Some researchers have recommended limited-spectrum antibiotics, while others prefer a broader-spectrum approach.13 Several recent studies14 have suggested that erythromycin is effective for eradicating Mycoplasma and Ureaplasma and beneficial for the neonate.
Optimal duration of antibiotic therapy is unclear
Most early studies advocated standard treatment from the time of ruptured membranes until delivery, while others recommended 7 to 10 days of therapy. Several recent trials15 have found 3 days of therapy to be equivalent to 7 days. However, these studies lack sufficient power to warrant a shorter duration of therapy at this time.
Numerous small, prospective, randomized trials comparing antibiotics with placebo have demonstrated prolonged latency (period from rupture of membranes to delivery) in the women with preterm premature rupture of membranes (PPROM) who were given antibiotics.
However, these studies lacked sufficient power to establish a decrease in neonatal morbidity with antibiotics, although a meta-analysis by Mercer and Arheart31 suggested such a decrease existed.
The breakthrough trial
Finally, in 1997, the Maternal-Fetal Medicine Network of the National Institute of Child Health and Human Development published a study large enough to definitively answer the question.12
A significant decrease in morbidity and mortality
Since these findings were published, controversy has shifted to the choice of antibiotics and the length and route of administration.
In this study, 614 women between 24 and 32 weeks of gestation with confirmed PPROM were randomized to intravenous ampicillin (2 g every 6 hours) and erythromycin (250 mg every 6 hours) for 48 hours followed by oral amoxicillin (250 mg every 8 hours) and erythromycin base (333 mg every 8 hours) for 5 days, or placebo. None of the women had received corticosteroids for fetal maturation or antibiotic treatment within 1 week of randomization.
In the study group, the composite primary outcome of interest decreased significantly—pregnancies with at least 1 of the following: fetal or infant mortality, respiratory distress, severe intraventricular hemorrhage, stage 2 or 3 necrotizing enterocolitis, or sepsis within 72 hours of birth.
Practice recommendation
I use ampicillin (2 g IV every 6 hours) and azithromycin (500 mg orally or IV on day 1 followed by 250 mg every day for 4 days) because data from the ORACLE trial14 suggested an increased incidence of necrotizing enterocolitis with amoxicillin and clavulanic acid. I also treat patients for 7 full days, even though preliminary data suggests 3 days may be adequate.15
More trials ahead
Expect to see many more randomized trials seeking to establish the best antibiotic, route of administration, and length of treatment.