Avoiding vascular injury at laparoscopy
An expert traces distances between trocar entry and vascular landmarks, describes the safest insertion techniques, and outlines decisive action in case of injuries.
Use a shorter insufflation needle
Our data on women with a BMI greater than 30 (obese range) indicate that the mean thickness of the anterior abdominal wall is 5.05 cm and the distance to the aorta is 15.14 cm.15 A standard Verres needle measures 12.5 cm from the tip of the shaft to the point where the shaft joins the hub of the needle. This is clearly excessive length, since women with a BMI above 30 have an abdominal wall thickness of approximately 5.05 cm and women with BMIs between 25 and 30 have a thickness of only 3.85 cm.
I prefer a Touhy epidural needle for subumbilical insertion and creation of the pneumoperitoneum, since it is a relatively short 8.5 cm. Thus, it is less hazardous than the Verres needle. It also is less likely to clog with tissue fragments because of its curved tip, and more likely to create a successful pneumoperitoneum on the first try.
Fortunately, large-vessel injuries caused by the insufflation needle are rare.
Proper insertion technique
I have residents draw a straight line with a marking pen from the lower margin of the umbilicus to the superior margin of the pubic symphysis. This serves as a guide to keep the trocar pointing toward the middle of the abdomen, away from the iliac vessels. I also teach residents to thrust the trocar in the midline at a 45° to 60° angle in relation to the plane of the abdominal wall, with the trocar pointing toward the uterus (FIGURES 2 AND 3).
Many residents twist disposable trocars during insertion. This “door knob” movement works against the design of the trocar and traumatizes tissue. The correct approach is thrusting the device into the abdominal cavity, or holding the trocar (only for disposable trocar devices) like a dart and thrusting it into the abdomen as though throwing a dart. The only trocar designed for twisting is the conical reusable device; the sharp pyramidal reusable trocar should be thrust rather than twisted.
Avoid “long” trocars
These are a full 5 cm longer than the 20-cm standard device (hub of handle to tip of shaft). Abdominal wall measurements indicate that these devices are never required to simply penetrate the anterior abdominal wall; these trocars also carry the risk of hitting the iliac vessels.
Open laparoscopy is not foolproof
Although open laparoscopy would seem to guarantee safe entry of the primary trocar, reports of aortic injuries have recently been published. Similar data have been reported for optical access trocars.11,18
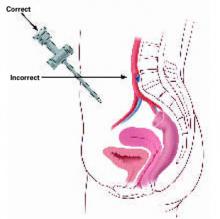
FIGURE 2 Insert the trocar at 45° to 60° angle
At insertion, the trocar should be at a 45°to 60°angle relative to the abdominal wall, with the tip of the device tilted in the direction of the uterus and bladder. A 90°angle of insertion is dangerous.
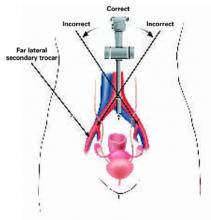
FIGURE 3 Midline insertion is safest
Insert the primary trocar in the midline pointing toward the uterus; deviation to the right or left is dangerous. Also avoid injuring the inferior epigastric and external iliac vessels with far lateral trocar insertion.
Body habitus and vascular injury
The obese patient of short stature is at the greatest risk for vascular injury. Although the relative distances between the anterior abdominal wall and the aorta are greater at the highest BMI levels, short stature means that the iliac vessels are closer. Significantly, large vessel injuries in the series cited herein were associated with the use of disposable trocars 90% of the time.
I believe high-risk conditions are created when carbon dioxide gas is inadvertently infused into the properitoneal fat space (FIGURE 4). As the volume of gas grows, the anterior wall parietal peritoneum dissects free from the remainder of the anterior abdominal fat, creating a pseudo-pneumoperitoneum. The operator fails to realize that the true peritoneal cavity has not been entered and, in fact, has paradoxically constricted in size because of the enlarging pseudoperitoneal space. Careful attention to the pressure gauges would have aroused suspicion that gas was being infused into the wrong space, since pressures tend to be higher and flow erratic in such situations.
Nevertheless, the surgeon places a trocar into the space, looks through the laparoscope, sees red or yellow, and realizes that the peritoneal cavity has not been entered. More gas is insufflated and the trocar is tried again.
Typically, the duller, reusable trocar pushes the leading edge of the peritoneum rather than penetrating it, further enlarging the properitoneal space and bringing the anterior and posterior peritoneal walls very close together.
In another scenario, the same set of circumstances exists except, rather than employing a reusable trocar, the surgeon selects a disposable device or even, after 2 failures to enter the peritoneal cavity with the reusable device, an extra-long (11-inch) disposable trocar (FIGURE 4).