Assessment of abnormal uterine bleeding: 3 office-based tools
Sophisticated, user-friendly tools now available for office diagnosis of dysfunctional bleeding are underutilized. Here, a thorough assessment of transvaginal ultrasound, saline-infusion sonography, and hysteroscopy.
Another investigation compared the accuracy and pain of SIS with flexible office hysteroscopy.14 For all findings combined—including polyps, submucous myomas, synechiae, endometrial hyperplasia, and cancer—SIS’s sensitivity was 96% and its specificity was 88%, compared with hysteroscopy. SIS did not miss any intracavitary lesions. It was also less painful than hysteroscopy. False-positive results included diagnosing endometrial polyps as fibroids or vice versa. This is not really a problem, however, since both lesions are associated with bleeding abnormalities and both are removed with the operative hysteroscope.
False-positive results may be caused by blood, debris, clots, thickened endometrial folds, secretory endometrium, detached fragments of endometrium, or endometrium that was sheared during placement of the catheter. (When SIS is performed in the presence of active uterine bleeding, endometrial clots may sometimes be mistaken for polyps, fibroids, or hyperplasia.)
Because false positives may lead to unnecessary surgical intervention,16 SIS should be performed when these are least likely. For premenopausal women, that means scheduling SIS within 1 to 7 days of the menstrual cycle’s completion. In postmenopausal women, the patient should be scanned when she is not bleeding, if possible. If she is taking sequential HRT, SIS is best performed after progesterone withdrawal.
Until insurers realize the advantages of office-based hysteroscopy and reimburse accordingly, women will be unnecessarily subjected to surgery, preoperative testing, lost time, and increased anxiety.
Some have suggested that if SIS detects a lesion smaller than 10 mm, the procedure should be repeated when the patient is not bleeding. If the lesion is still present, operative intervention is appropriate.17,18
Cost issues. The development of clinical algorithms incorporating SIS—particularly those that take into account the differences between evaluation of premenopausal and postmenopausal women—may decrease costs by eliminating unnecessary D&Cs and endometrial biopsies, including those that are hysteroscopically directed.
For example, a study examining almost 1,200 women in 4 Nordic countries suggests that in women with postmenopausal bleeding and an endometrial thickness of 4 mm or less, curettage is unnecessary.19 An algorithm developed after the evaluation of more than 400 perimenopausal women concluded that hysteroscopically directed endometrial biopsy is best for women with focal processes, while endometrial aspiration biopsy is best for those with global disease.20
Although SIS overcomes many of the limitations of TVUS, in some cases the endometrium simply cannot be visualized.
In general, SIS is less costly to perform than hysteroscopy.
For a successful surgical outcome, it is important to preoperatively identify the size, number, location, and depth of intramural extension. Fibroid size and location affect resectability, the number of surgical procedures necessary for complete resection, the duration of surgery, and the potential complications from fluid overload.1
Using saline-infusion sonography (SIS), uterine fibroids can be categorized into 3 classes. An experienced surgeon can successfully resect class 1 (FIGURE 1) or class 2 (FIGURE 2) fibroids hysteroscopically. Class 3 fibroids (FIGURE 3) are less amenable to such surgery because perforation is a significant risk. Fluid overload, contracture of the endometrial cavity, and incomplete resection also are possible complications.2
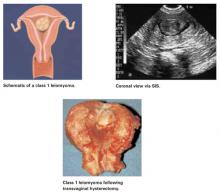
FIGURE 1 Class 1 fibroids
Class 1 fibroids occur completely within the uterine cavity, with no involvement of myometrium. The base or stalk is visible with SIS.
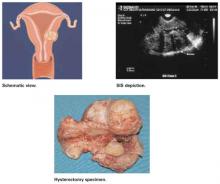
FIGURE 2 Class 2 fibroids
Class 2 fibroids have a submucosal component involving less than half of the myometruim.
FIGURE 3 Class 3 fibroids
Class 3 fibroids have an intramural component of greater than 50%. They can be transmural, and may be located anywhere from the submucosa to the serosa. These fibroids often appear as a bulge or indentation into the submucosa.
REFERENCES
1. Emanuel MH, Verdel MJ, Wamsteker K. A prospective comparison of transvaginal ultrasonography and diagnostic hysteroscopy in the evaluation of patients with abnormal uterine bleeding: Clinical implications. Am J Obstet Gynecol. 1995;172:547-552.
2. Bradley LD, Falcone T, Magen AB. Radiographic imaging techniques for the diagnosis of abnormal uterine bleeding. Obstet Gynecol Clin North Am. 2000;27:245-276.
Office hysteroscopy
Hysteroscopy has revolutionized the practice of gynecology. Thanks to improvements in optics and subsequent reduction in hysteroscope diameters in the 1980s and 1990s, office use has become practical. Thin operative hysteroscopes with outer diameters ranging from 3 mm to 5 mm now are available. A study in 417 women undergoing flexible hysteroscopy in an office setting without anesthesia demonstrated the patient acceptability, diagnostic accuracy, and cost-effectiveness of this technology.21
Advantages of hysteroscopic visualization include:
- immediate office evaluation
- direct visualization of the endometrium and endocervix
- the ability to detect minute focal endometrial pathology
- the ability to perform directed endometrial biopsies (with some hysteroscopes) and lyse filmy adhesions with the distal tip of the flexible hysteroscope22