Endometrial ablation: a look at the newest global procedures
With the recent FDA approval of cryoablation, bipolar desiccation, and hydrothermal ablation, Ob/Gyns have more options for the quick, simple, and effective treatment of menorrhagia.
Cost. The disposable cryoprobes are $1,250 per case, and the unit costs $29,995. Since most ablation procedures currently are performed in the operating room, ancillary costs of the techniques are similar.
Bipolar desiccation
Technique. After dilating the cervix, insert the 8-mm NovaSure System (Novacept, Palo Alto, Calif) catheter into the uterus. To rule out auterine perforation prior to beginning the procedure, insert carbon dioxide (CO2) into the cavity (Figure 4).The machine will not turn on if a seal of CO2 has not been created, unless the surgeon overrides the system.
Then expand the 3-dimensional gold-plated bipolar mesh electrode, which imitates the shape of the uterine cavity, out of the catheter. Gently push the probe toward the fundus so that the mesh electrode is accurately positioned within the uterine cavity (Figure 5). Once the electrode is activated with up to 180 W of bipolar power, gentle suction brings the endometrium into close contact with the mesh (Figure 6). This suction also removes debris and allows for more complete desiccation.
The entire bipolar desiccation procedure takes less than 5 minutes to perform.
The system shuts down automatically when complete desiccation (calculated at 50 ohms of resistance) has occurred. The average treatment time is just over 1 minute, and the average depth of ablation is 4 to 5 mm.9 Once ablation is complete, retract the mesh electrode and remove the catheter (Figure 7). The entire procedure takes less than 5 minutes.
Advantages. Not only is the technique quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
Disadvantages. There are limited data on the 1-year success rates for this completely blind procedure. In addition, the uterus needs to be of normal shape to successfully ablate the endometrium.
What the evidence shows. Unpublished data from randomized, controlled clinical trials comparing bipolar desiccation with balloon ablation have demonstrated that the former achieves higher amenorrhea and success (a return to normal menstrual bleeding) rates than the latter. Further, patients treated with bipolar desiccation experienced less pain, both intra-operatively and postoperatively, than women who underwent balloon ablation.
Cost. Each disposable probe costs $850, and the bipolar controller lists for $15,000.
FIGURE 4
Dilate the cervix and insert the 8-mm catheter. To rule out a uterine perforation prior to beginning the procedure, place carbon dioxide in the cavity.
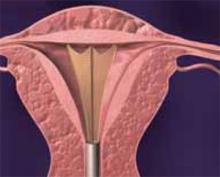
FIGURE 5
Expand the bipolar mesh electrode. Gently push the probe toward the fundus to accurately position the electrode within the uterine cavity.
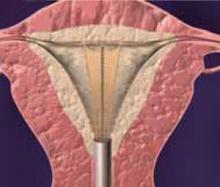
FIGURE 6
Activate the electrode with up to 180 W of bipolar power. A gentle suction brings the endometrium into close contact with the mesh.
FIGURE 7
The system shuts down automatically when complete desiccation has occurred. Retract the bipolar mesh electrode and remove the catheter.
Hydrothermal ablation/circulating heated saline
Technique. Begin by dilating the cervix and inserting the sheath, which includes an 8-mm hysteroscope (Hydro ThermAblator; BEI Medical Systems, Teterboro, NJ), into the uter-ine cavity. Using gravity rather than a pump, introduce saline solution through the sheath into the uterus. As the saline circulates, gradually heat it until the solution reaches and maintains 90 degrees Celsius for 10 minutes, completely destroying the endometrium. (The total time from insertion of the sheath to completion of the procedure is 17 minutes.)
A safety feature detects whether any fluid has escaped from the closed system; a shutoff mechanism activates if more than 10 cc of fluid are lost. The system is controlled by software, so even physicians who are inexperienced with hysteroscopy can easily perform this technique.
Advantages. The primary advantage of hydrothermal ablation (HTA) is that the circulating hot saline solution contacts the entire endometrial surface regardless of the size or shape of the uterine cavity. In addition, since the procedure is performed under direct visualization, the surgeon can ensure that the entire cavity has been thoroughly ablated.
Disadvantages. One drawback is that it can be a painful procedure because the hysteroscope is large, necessitating wide dilation of the cervix, and hot water stimulates pain. Further, there have been unpublished reports of vaginal burns when the cervix created a poor seal around the sheath.
What the evidence shows. Based on their research of 276 women (187 women in the HTA group and 89 patients in the rollerball group), investigators have found that HTA has a treatment success rate of 77% compared to 82% for rollerball ablation. (The treatment success rate is defined as a PBAC score of 75 or lower; eumenorrhea is a score of less than 100.) Amenorrhea rates at 12-month follow-up were 40% and 51%, respectively. The researchers concluded that HTA offers an advantage over rollerball ablation in that it reduces anesthesia requirements and eliminates the problem of hypotonic fluid absorption.10