Vulvar pain syndromes: Causes and treatment of vestibulodynia
Although the origins of vestibulodynia are incompletely understood, this subset of vulvar pain is manageable and—good news—even curable in some cases
IN THIS ARTICLE
Dr. Haefner: The response to treatment in many pain patients depends on the amount of time that the pain has been present. Someone who has had pain for 30 years will probably not be cured 3 months after starting treatment. However, someone with a short duration of pain often gets good improvement. One hundred percent improvement is rare, however. Many patients are able to approach the 80% improvement mark.
Dr. Edwards: I would say that these conditions are manageable more than curable, although pure vestibulodynia—which is uncommon—is curable with surgery.
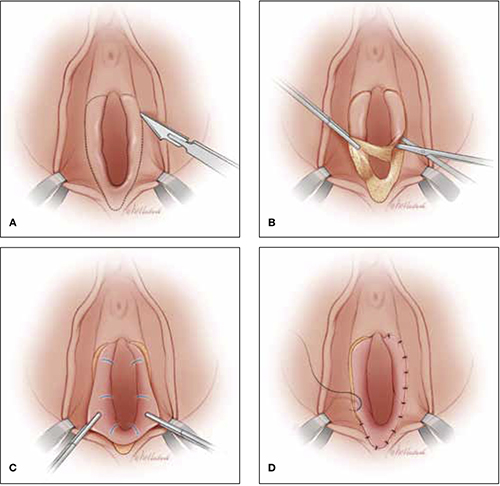
Vestibulectomy technique
(A) Incision. In many cases, the incision needs to extend up to the opening of the Skene’s ducts on the vestibule before it is carried down laterally along Hart’s line to the perianal skin, with the mucosa undermined above the hymeneal ring. (B) Excision. Remove the tissue superior to the hymeneal ring. (C) Advancement of vaginal mucosa. Further undermine the mucosa and advance it to close the defect. (D) Suturing. Close the defect in two layers using absorbable suture.
Is vestibulectomy definitive treatment?
Dr. Lonky: Does vestibulectomy work as a definitive treatment for PVD?
Dr. Gunter: Vestibulectomy—that is, resection of the vestibule and advancement of vaginal mucosa—is well described for women who have localized vestibulodynia. The complication rate is low, with only 3% of women reporting worsening of symptoms after the procedure.19,20 Success rates range from 17% to 89%, although many studies are retrospective reviews or include nonhomogenous populations, or both.19–21 A prospective study (Level II) indicates a 52% reduction in pain scores for women 6 months after vestibulectomy—and the scores continued to improve at evaluation at 2.5 years.22,23
Prospective studies indicate that vestibulectomy improves pain scores more than cognitive behavioral therapy, biofeedback, oral despiramine, and topical lidocaine.22,23 However, even surgery carries a robust placebo response rate, and vulvar biopsy alone has been associated with an improvement in pain scores in 67% of women.24,25
I offer surgery for vestibulodynia after the patient has failed at least two therapies (two topical treatments or one topical and one oral treatment). I offer injections before proceeding, and almost all patients opt to try them. I do not offer vestibulectomy to patients who have unprovoked pain or pain outside of resection margins.
Dr. Haefner: Surgical excision of the vulvar vestibule has met with success, in some studies, in more than 80% of cases, but it should be reserved for women who have longstanding and localized vestibular pain in whom other management options have failed.
The patient should undergo cotton-swab testing to outline areas of pain before anesthesia is administered in the operating room. Often, the incision will need to extend up to the opening of the Skene’s ducts on the vestibule (FIGURE). The incision is carried down laterally along Hart’s line to the perianal skin, and the mucosa is undermined above the hymeneal ring. The specimen is excised superior to the hymeneal ring. The vaginal tissue is further undermined and brought down to close the defect in two layers using absorbable suture. A review of this technique with illustrations has been published.26
Dr. Lonky: Thank you all again for sharing your considerable expertise, experience, and insight.
Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58(2):82–88.
In this population-based study, 16% of women reported a history of chronic unexplained vulvar pain, and nearly 7% reported current symptoms.
Khandker M, Brady SS, Vitonis AF, Maclehose RF, Stewart EG, Harlow BL. The influence of depression and anxiety on risk of adult onset vulvodynia [published online ahead of print August 8, 2011].
J Womens Health (Larchmt). doi:10.1089/jwh.2010.2661.
Vulvodynia was four times more likely among women who had antecedent mood or anxiety disorders than in women who didn’t. Vulvodynia was also associated with new or recurrent onset of mood or anxiety disorders.
Masheb RM, Wang E, Lozano C, Kerns RD. Prevalence and correlates of depression in treatment-seeking women with vulvodynia. J Obstet Gynaecol. 2005;25(8):786–791.
Comorbid major depressive disorders in women who have vulvodynia are related to greater pain severity and worse functioning.
Reed BD, Haefner HK, Punch MR, Roth RS, Gorenflo DW, Gillespie BW. Psychosocial and sexual functioning in women with vulvodynia and chronic pelvic pain. A comparative evaluation. J Reprod Med. 2000;45(8):624–632.
Women who have vulvodynia are psychologically similar to women who don’t. A primary psychological cause of vulvodynia is not supported.
Tribo MJ, Andion O, Ros S, et al. Clinical characteristics and psychopathological profile of patients with vulvodynia: an observational and descriptive study. Dermatology. 2008;216(1):24–30.
Psychiatric treatment may be a useful option to improve symptoms of vulvodynia.










