Your 15-year-old patient requests an IUD without parental knowledge
The dilemmas of adolescent consent
General requirements of consent
Even when adolescent consent is permitted for treatment, including in cases of contraception, it is essential that all of the legal and ethical requirements related to informed consent are met.
1. The adolescent has the capacity to consent. This means not only that the state-mandated requirements are met (age, for example) but also that the patient can and does understand the various elements of consent, and can make a sensible, informed decision.
The bottom line is “adolescent capacity is a complex process dependent upon the development of maturity of the adolescent, degree of intervention, expected benefit of the medical procedure, and the sociocultural context surrounding the decision.”11 Other items of interest include the “evolving capacity” of the child,12 which is the concept of increasing ability of the teen to process information and provide more appropriate informed consent. Central nervous system (CNS) maturation allows the adolescent to become increasingly more capable of decision making and has awareness of consequences of such decisions. Abstract thinking capabilities is a reflection of this CNS maturing process. If this competency is not established, the adolescent patient cannot give legitimate consent.
,2. The patient must be given appropriate information (be “informed”). The discussion should include information relevant to the condition being treated (and the disease process if relevant). In addition, information about the treatment or intervention proposed and its risks and alternatives must be provided to the patient and in a way that is understandable.
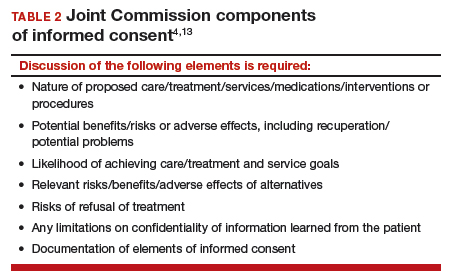
3. As with all patients, consent must be voluntary and free of coercion or manipulation. These elements of informed consent are expanded on by the Joint Commission, which has established a number of components of informed consent (TABLE 2).4,13
Confidentiality and release of information to parents and others
Similar to consent, parents historically have had the authority to obtain medical information about their minor children. This right generally continues today, with some limitations. The right to give consent generally carries with it the right to medical information. There are some times when parents may access medical information even if they have not given consent.
This right adds complexity to minor consent and is an important treatment issue and legal consideration because confidentiality for adolescents affects quality of care. Adolescents report that “confidentiality is an important factor in their decision to seek [medical] care.”14 Many parents are under the assumption that the health care provider will automatically inform them independent of whether or not the adolescent expressed precise instruction not to inform.15,16
Of course if a minor patient authorizes the physician to provide information to her parents, that is consent and the health care provider may then provide the information. If the patient instructs the provider to convey the information, the practitioner would ordinarily be expected to be proactive in providing the information to the parent. The issue of “voluntariness” of the waiver of confidentiality can be a question, and the physician may discuss that question with the patient. Ordinarily, however, once a minor has authorized disclosure to the parent, the clinician has the authority to disclose the information to the parent, but not to others.
All of the usual considerations of confidentiality in health care apply to adolescent ObGyn services and care. This includes the general obligation not to disclose information without consent and to ensure that health care information is protected from accidental release as required by the Health Insurance Portability and Accountability Act (HIPAA) and other health information privacy laws.17
It is important to emphasize that the issues of consent to abortion are much different than those for contraception and sexually transmitted infections. As our case presentation does not deal with abortion, we will address this complex but important discussion in the future--as there are an estimated 90,000 abortions in adolescent girls annually.1
Given that abortion consent and notification laws are often complex, any physician providing abortion services to any minor should have sound legal advice on the requirements of the pertinent state law. In earlier publications of this section in OBG Management we have discussed the importance of practitioners having an ongoing relationship with a health law attorney. We make this point again, as this person can provide advice on consent and the rights of parents to have information about their minor children.
Reference
- Henshaw SK. U.S. teenage pregnancy statistics with comparative statistics for women age 20-24. New York, New York: Alan Guttmacher Institute; May 2003.
Continue to: How and when to protect minor confidentiality...








