2016 Update on fertility
Too many women and men around the world are affected by infertility. Unfortunately, access to assisted reproduction therapies (ART) when necessary is not balanced. These experts address how natural fertility can be optimized and why efforts to address ART access barriers are needed.
In this Article
- Factors affecting the probability of conception
- Barriers to ART access
- Ways to increase ART funding
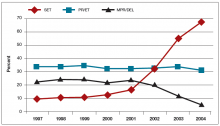
This government mandate changes clinical practice toward maximizing pregnancy rates because IVF clinics cannot afford, for competitive reasons, to have lower pregnancy rates than other clinics. This is unfortunate, because it has been shown that when elective single embryo transfer (eSET) is implemented, pregnancy rates do not decrease significantly but, in fact, multiple pregnancy rates drop dramatically (FIGURE 2).23
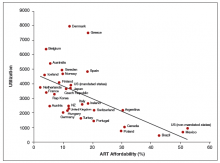
The cost of IVF obviously impacts access, but the issue is more complex than it appears. IVF in the United States costs about 30% to 50% more than in other countries. But general US health care costs are also relatively even higher than that, and IVF is not expensive relative to other medical services.24,25 Nevertheless, compared with other countries, the average US cost of a standard fresh IVF cycle is the highest as a percentage of gross national income per capita, at about 25%.26 However, because of higher live birth rates, the cost-effectiveness of ART (which is the cost per live birth) in the United States is not unfavorable relative to other countries.26
What matters to patients, however, is affordability, which is the net cost to patients after all subsidies relative to disposable income. US out-of-pocket costs for IVF as a percent of annual disposable income make IVF costs in the United States among the least affordable in the world. Affordability predicts utilization, as well as number of embryos transferred.24 It is clear that less affordable IVF cycles result in more embryos being transferred. Broad insurance mandates result in large increases in treatment access but also significantly less aggressive treatment. More limited insurance mandates generally have little effect on IVF markets, which is why there is only a slight difference in practice behavior in mandated states because, nationally, coverage is poor (FIGURE 3).24,27,28
We must increase access to ART by increasing funding
In summary, the economic factors that affect affordability are the cost of treatment, socioeconomic status, disposable income, government coverage, insurance coverage, and access to financing/loan programs. Access is affected by many factors, but only countries with funding arrangements that minimize out-of-pocket expenses meet expected demand of infertile patients. ART is expensive from a patient perspective, but not from a societal perspective. To increase subsidies we must:
- change societal attitudes toward infertility
- change payor attitudes toward reproductive care
- convince payers of cost-effectiveness
- develop effective payment plans and programs
- improve protocols (eg, eSET)
- educate patients and professionals
- use technology appropriately
- standardize treatments through research
- innovate new technologies to reduce costs
- develop patient criteria for inclusion in subsidization.
The ASRM has taken the lead in this respect in the United States by having an Access to Care Summit in September 2015, as well as an Advocacy Forum, and will continue to advocate for better coverage for infertility care. Internationally, FIGO (the International Federation of Gynecologyand Obstetrics) has taken the initiative to increase ART access, with the Committee on Reproductive Medicine distributing The FIGO Fertility Toolbox (https://www.fertilitytool.com).
World Health Organization Infertility Initiative
The World Health Organization (WHO) has, over the past 5 years, made a major initiative to increase global access to infertility diagnosis and treatment. This effort was effected through 3 major activities:
- rapid assessment task force
- reproductive medicine glossary
- fertility guidelines.
The Rapid Assessment Task Force. This Task Force developed a comprehensive questionnaire for the 195 governments that belong to and adhere to WHO guidelines. This questionnaire, which is to be completed by government health departments, requires the government to document the breadth and depth of their infertility services and identify deficiencies or gaps. It is expected that the questionnaire will be distributed to all governments of the world in 2016, including the United States. The information that is received by the Task Force will be analyzed by the WHO to help develop plans for improved national infertility services globally.
The Reproductive Medicine glossary. This glossary being developed is a revision and major update of The International Committee Monitoring ART (ICMART)/WHO Glossary.29 The number of definitions in the glossary is being increased 4-fold to about 300 definitions to include not only ART but also sections on clinical definitions, out‑comes, laboratory/embryology, epidemiology/public health, and andrology. While easy to overlook, definitions are essential to the accurate documentation of disease, communication among professionals, research comparisons, insurance coverage, billing and coding, and other issues.
For example, because the definition of infertility must include not only couples but also single persons, be flexible to deal with clinical versus epidemiologic and public health requirements, account for pre-existing conditions and age, and identify it as both a disease and a disability. Abortion definitions are complicated by the desire of many to call spontaneous abortion “miscarriage” and by the duration of pregnancy necessary before “delivery” of a fetus occurs. There is a desire to remove conception as a term (although it is widely used) because it is not a biological event. Pregnancy has its own complexities, including when it is initiated, which is now considered to be at the time of implantation. The glossary is expected to be published by mid-2016.
The WHO infertility guidelines. These have been an exhaustively-developed set of guidelines based on a comprehensive review and assessment of the entire literature by approximately 60 international experts working in teams with other assistants and experts using a standardized PICO (Population, Intervention, Comparators, and Outcomes of interest) system. This was a truly herculean effort. Guidelines are being finalized in the following areas: female infertility, unexplained infertility, polycystic ovary syndrome, ovarian stimulation, intrauterine insemination, ovarian hyperstimulation syndrome, IVF, and male infertility. After thorough review by the WHO, these guidelines will be published in hard copy and electronically in mid-2016.
Watch for access tools available this year
The plans are for the Task Force recommendations, the glossary, and the fertility guidelines, including The FIGO Fertility Toolbox to be presented as a comprehensive package to all of the governments of the world in 2016. This will give them the tools and encouragement to assess their fertility services and to use the WHO fertility package to improve access, effectiveness, and safety of infertility services in their respective countries.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.