Ready to Go Home? Assessment of Shared Mental Models of the Patient and Discharging Team Regarding Readiness for Hospital Discharge
BACKGROUND: A critical task of the inpatient interprofessional team is readying patients for discharge. Assessment of shared mental model (SMM) convergence can determine how much team members agree about patient discharge readiness and how their mental models align with the patient’s self-assessment.
OBJECTIVE: Determine the convergence of interprofessional team SMMs of hospital discharge readiness and identify factors associated with these assessments.
DESIGN: We surveyed interprofessional discharging teams and each team’s patient at time of hospital discharge using validated tools to capture their SMMs.
PARTICIPANTS: Discharge events (n = 64) from a single hospital consisting of the patient and their team (nurse, coordinator, physician).
MEASURES: Clinician and patient versions of the validated Readiness for Hospital Discharge Scales/Short Form (RHDS/SF). We measured team convergence by comparing the individual clinicians’ scores on the RHDS/SF, and we measured team-patient convergence as the absolute difference between the Patient-RHDS/SF score and the team average score on the Clinician-RHDS/SF.
RESULTS: Discharging teams assessed patients as having high readiness for hospital discharge (mean score, 8.5 out of 10; SD, 0.91). The majority of teams had convergent SMMs with high to very high interrater agreement on discharge readiness (mean r*wg(J), 0.90; SD, 0.10). Yet team-patient SMM convergence was low: Teams overestimated the patient’s self-assessment of readiness for discharge in 48.4% of events. We found that teams reporting higher-quality teamwork (P = .004) and bachelor’s level–trained nurses (P < .001) had more convergent SMMs with the patient.
CONCLUSION: Measuring discharge teams’ SMM of patient discharge readiness may represent an innovative assessment tool and potential lever to improve the quality of care transitions. Journal of Hospital Medicine 2020;15:XXX-XXX.
© 2020 Society of Hospital Medicine
Prediction Models
For the exploratory aim, we first examined the bivariate relationship between the outcome variables (discharge teams’ assessment of patient readiness, team convergence, and team-patient convergence) and the identified contextual variables. We also checked for potential collinearity among the explanatory variables. Then we used a linear stepwise regression procedure to identify factors associated with each continuous outcome variable. Due to the small sample size, we performed separate backward stepwise regression selection analyses for the three outcomes of interest. The candidate explanatory variables were evaluated using P < .20 for model entry. Final models were evaluated using leave-one-out cross validation. STATA (v.15.1, StataCorp; 2017) was used for analysis.
RESULTS
Sample
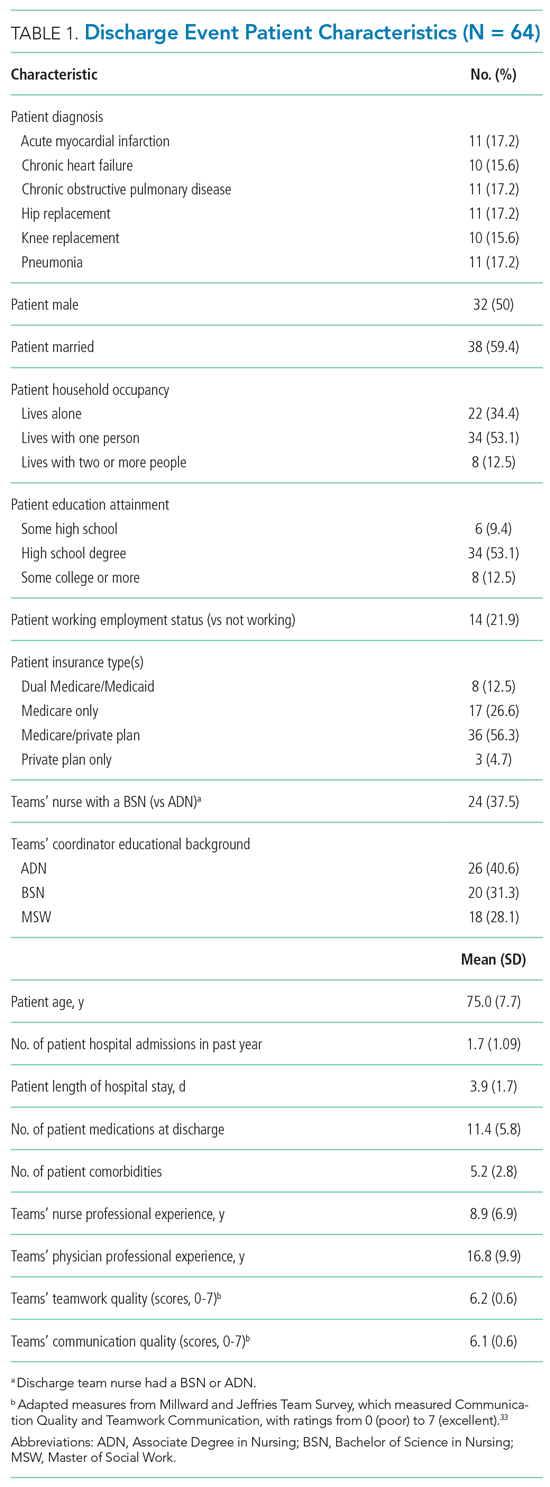
A total of 64 discharge events were included in this study. All discharge teams had a unique composition including 64 patients and varying combinations of 56 individual nurses (n = 27), physicians (n = 23), and coordinators (n = 6). Each event had three team members (ie, a nurse, a coordinator, and a physician) with no missing data. The majority of the 64 patient participants were White, retired, had a high school education, and lived in their own home with only one other person (Table 1).
Interprofessional Teams’ SMM of Readiness for Hospital Discharge
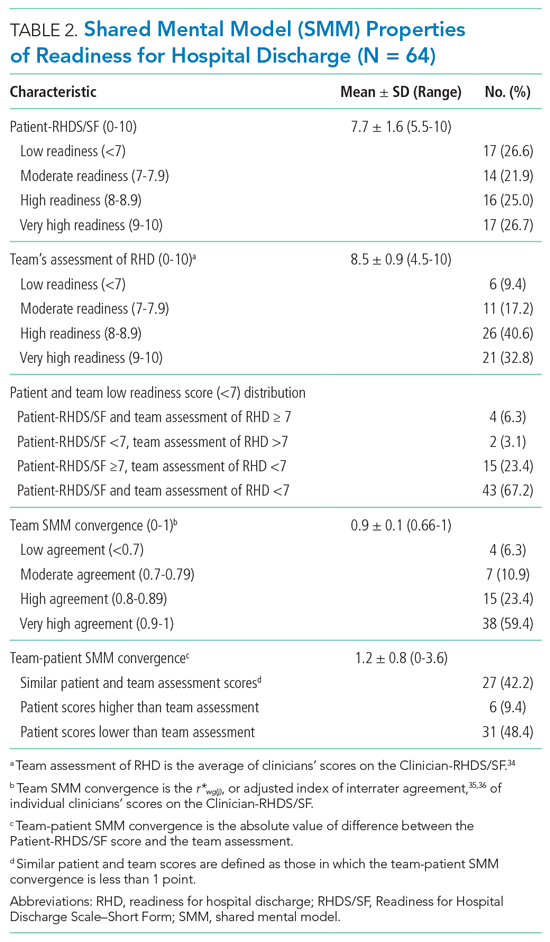
While the majority of teams perceived patients had high readiness for hospital discharge (mean, 8.5 out of 10; SD, 0.91), patients scores were nearly a full point lower (mean, 7.7; SD, 1.6; Table 2). The largest difference across categories was in the low-readiness category with 27% of patient scores falling into this category vs only 9.4% of discharge team mean scores. The mean SMM convergence of team perception of patients’ readiness for discharge was 0.90 (SD, 0.10); however, scores ranged from 0.66 (low agreement) to 1 (complete agreement). The average SMM team-patient convergence, or the discrepancy between the discharge team mean scores and the patient total scores across domains, was 1.16 (SD, 0.82). Of the 64 discharge events, 42.2% had similar team-patient perceptions of readiness for discharge, 9.4% had the patient reporting higher readiness for discharge than the team, and 48.4% had a team assessment rating of higher readiness for discharge than the patient’s self-assessment.
Prediction Models
In the exploratory analysis, we created individual linear regression models to predict the teams’ assessment, team convergence, and team-patient convergence for readiness of hospital discharge (Table 3; Appendix E). Factors associated with the teams’ assessment of discharge readiness included whether the patient was married and had less cognitive impairment, both of which were positively related to a higher-rated readiness among teams. An important system factor was higher quality of communication among team members, which was positively associated with teams’ assessment of patient discharge readiness. In contrast, only patient factors—married patients and those with a principal diagnosis of heart failure—were associated with more convergent team SMMs. Team-patient convergence was positively associated with two patient factors: marital status (married) and fewer comorbidities. However, team-patient convergence was also associated with two system factors: teams with a bachelor’s level–trained nurse (compared with a nurse with an associate degree ) and teams reporting a higher quality of teamwork on day of discharge.