Ready to Go Home? Assessment of Shared Mental Models of the Patient and Discharging Team Regarding Readiness for Hospital Discharge
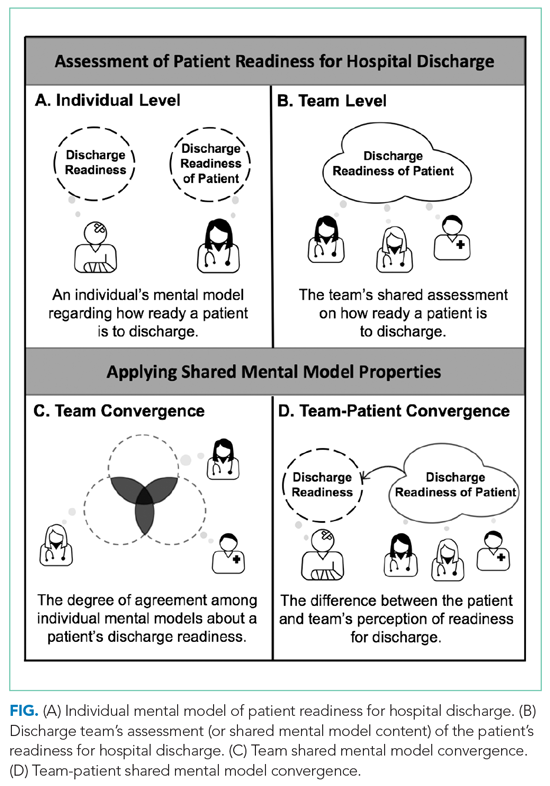
BACKGROUND: A critical task of the inpatient interprofessional team is readying patients for discharge. Assessment of shared mental model (SMM) convergence can determine how much team members agree about patient discharge readiness and how their mental models align with the patient’s self-assessment.
OBJECTIVE: Determine the convergence of interprofessional team SMMs of hospital discharge readiness and identify factors associated with these assessments.
DESIGN: We surveyed interprofessional discharging teams and each team’s patient at time of hospital discharge using validated tools to capture their SMMs.
PARTICIPANTS: Discharge events (n = 64) from a single hospital consisting of the patient and their team (nurse, coordinator, physician).
MEASURES: Clinician and patient versions of the validated Readiness for Hospital Discharge Scales/Short Form (RHDS/SF). We measured team convergence by comparing the individual clinicians’ scores on the RHDS/SF, and we measured team-patient convergence as the absolute difference between the Patient-RHDS/SF score and the team average score on the Clinician-RHDS/SF.
RESULTS: Discharging teams assessed patients as having high readiness for hospital discharge (mean score, 8.5 out of 10; SD, 0.91). The majority of teams had convergent SMMs with high to very high interrater agreement on discharge readiness (mean r*wg(J), 0.90; SD, 0.10). Yet team-patient SMM convergence was low: Teams overestimated the patient’s self-assessment of readiness for discharge in 48.4% of events. We found that teams reporting higher-quality teamwork (P = .004) and bachelor’s level–trained nurses (P < .001) had more convergent SMMs with the patient.
CONCLUSION: Measuring discharge teams’ SMM of patient discharge readiness may represent an innovative assessment tool and potential lever to improve the quality of care transitions. Journal of Hospital Medicine 2020;15:XXX-XXX.
© 2020 Society of Hospital Medicine
METHODS
Design
We used a cross-sectional survey design at a single Midwestern community hospital to determine inpatient care teams’ SMMs of patient hospital discharge readiness. This study is part of a larger mixed-methods evaluation of interprofessional hospital discharge teamwork in older adult patients at risk for a poor transition to home.9 Data were collected using questionnaires from patients and their team (nurse, coordinator, and physician) within 4 hours of the patient leaving the hospital. First, we measured the teams’ assessment, team convergence, and team-patient convergence on patient readiness for discharge from the hospital. Then, after identifying relevant potential predictors from the literature, we developed regression models to predict the teams’ assessment, team convergence, and team-patient convergence of discharge readiness based on these variables. Our local institutional review board approved this study.
Sample and Participants
We used a convenience sampling approach to identify eligible discharge events consisting of the patient and care team.9 We focused on patients at high-risk for poor hospital-to-home transitions.3,22 Eligible events included older patients (≥65 years) who were discharged home without home health or hospice services and admitted with a primary diagnosis of heart failure, acute myocardial infarction, hip replacement, knee replacement, pneumonia, or chronic obstructive pulmonary disease. Patient exclusion criteria included inability to complete study forms because of mental incapacity or a language barrier. Discharge team member inclusion criteria included the bedside nurse, attending physician, and coordinator (a unit-dedicated discharge nurse or social worker) caring for the patient participant at the time of hospital discharge. Each discharge team was unique: The same three individuals could not be included as a “team” for more than one discharge event, although individual members could be included as a part of other teams with a different set of individuals. Appendix A provides an enrollment flowchart.
Conceptual Framework
We applied the SMM conceptual framework to the context of hospital discharge. As shown in the Figure, SMMs are examined at the team level and contain the critical knowledge held by the team to be effective.15,16 From a patient-centered perspective, patients are considered the expert on how ready they feel to be discharged home.20,23,24 In this case, the SMM content is the discharge team members’ shared assessment of how ready the patient is for hospital discharge (Figure, B).10 Convergence is the degree of agreement among individual mental models.10-13 In this study we examined two types of convergence: (1) team convergence, or the team members degree of agreement on the patient’s readiness for discharge (Figure, C), and (2) team-patient convergence, or the degree to which the team’s SMM aligns with the patient’s mental model (Figure, D).10-13
Measures and Variables
Readiness for Hospital Discharge Scales/Short Form
We used parallel clinician and patient versions of the Readiness for Hospital Discharge Scale/Short Form (RHDS/SF)25-28 to determine the teams’ assessment of discharge readiness, team SMM convergence, and team-patient SMM convergence.
The RHDS/SF scales are 8-item validated instruments that use a Likert scale (0 for not ready to 10 for totally ready) to assess the individual clinician’s or patient’s perceptions of how ready the patient is to be discharged.20,25,27 The RHDS/SF instruments include four dimensions conceptualized as crucial to patient readiness for discharge and important to anticipatory planning: (1) Personal Status, physical-emotional state of the patient before discharge; (2) Knowledge, perceived adequacy of information needed to respond to common posthospitalization concerns/problems; (3) Coping Ability, perceived ability to self-manage health care needs; and (4) Expected Support, emotional-physical assistance available (Appendix B).20,25,27 The RHDS/SF instruments’ results are calculated as a mean of item scores, with higher individual scores indicating the rater assessed the patient as being more ready for hospital discharge.20 The RHDS/SF scales have undergone rigorous psychometric testing and are linked to patient outcomes (eg, readmissions, emergency room visits, patient coping difficulties after discharge, and patient-rated quality of preparation for posthospital care).20,25-28 For example, predictive validity assessments for adult medical-surgical patients found lower Nurse-RHDS/SF scores are associated with a six- to ninefold increase in 30-day readmission risk.20