Reducing Unnecessary Treatment of Asymptomatic Elevated Blood Pressure with Intravenous Medications on the General Internal Medicine Wards: A Quality Improvement Initiative
BACKGROUND: Asymptomatic elevated blood pressure (BP) is common in the hospital. There is no evidence supporting the use of intravenous (IV) antihypertensives in this setting.
OBJECTIVE: To determine the prevalence and effects of treating asymptomatic elevated BP with IV antihypertensives and to investigate the efficacy of a quality improvement (QI) initiative aimed at reducing utilization of these medications.
DESIGN: Retrospective cohort study.
SETTING: Urban academic hospital. PATIENTS: Patients admitted to the general medicine service, including the intensive care unit (ICU), with ≥1 episode of asymptomatic elevated BP (>160/90 mm Hg) during hospitalization.
INTERVENTION: A two-tiered, QI initiative.
MEASUREMENTS: The primary outcome was the monthly proportion of patients with asymptomatic elevated BP treated with IV labetalol or hydralazine. We also analyzed median BP and rates of balancing outcomes (ICU transfers, rapid responses, cardiopulmonary arrests).
RESULTS: We identified 2,306 patients with ≥1 episode of asymptomatic elevated BP during the 10-month preintervention period, of which 251 (11%) received IV antihypertensives. In the four-month postintervention period, 70 of 934 (7%) were treated. The odds of being treated were 38% lower in the postintervention period after adjustment for baseline characteristics, including length of stay and illness severity (OR = 0.62; 95% CI 0.47-0.83; P = .001). Median SBP was similar between pre- and postintervention (167 vs 168 mm Hg; P = .78), as were the adjusted proportions of balancing outcomes.
CONCLUSIONS: Hospitalized patients with asymptomatic elevated BP are commonly treated with IV antihypertensives, despite the lack of evidence. A QI initiative was successful at reducing utilization of these medications.
© 2019 Society of Hospital Medicine
Among patients treated with IV antihypertensive medications, we compared the proportion of pretreatment SBPs falling into each of three specified ranges (SBP <180 mm Hg, SBP 180-199 mm Hg, and SBP >200 mm Hg) between baseline and intervention periods using chi-squared tests.
Using aggregate data, we compared the unadjusted proportion of patients treated with IV antihypertensive medications between pre- and postintervention periods using a chi-squared test. Next, using patient-level data, a logistic regression analysis was performed to examine the association between receipt of IV antihypertensive medications and time (dichotomized between pre- and postintervention periods) while adjusting for age, sex, race, ethnicity, primary language, insurance status, preexisting HTN, length of stay, and APR-DRG weight.
Rates of balancing outcomes were compared using chi-squared tests. A logistic regression analysis using patient-level data was also performed to investigate the association between each of these outcomes and the intervention period (pre vs post) while adjusting for age, sex, race, ethnicity, primary language, insurance status, preexisting HTN, length of stay, and APR-DRG weight.
RESULTS
Baseline Period
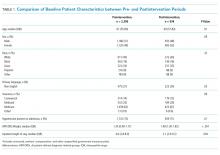
We identified 2,306 patients with ≥1 episode of asymptomatic elevated BP during the 10-month preintervention period. Patients on average experienced 9 episodes of elevated BP per hospitalization, representing 21,207 potential opportunities for treatment. Baseline characteristics are summarized in Table 1. In general, this represents an older population that was medically complex and multiracial.
Of these patients, 251 (11%) received IV hydralazine and/or labetalol at least once during their hospitalization, with a total of 597 doses administered. Among those treated, a median of 2 doses were given per patient (IQR: 1-4), 64% of which were hydralazine. The majority (380 [64%]) were ordered on an “as needed” basis, while 217 (36%) were administered as a one-time dose. Three-quarters of all doses were ordered by the teaching service (456 [76%]), with the remaining 24% ordered by the direct-care (hospitalist) service.
During the baseline period among patients receiving IV antihypertensive medications, the median SBP of the population prior to treatment was 187 mm Hg (IQR 177-199; Table 2). Treatment was initiated in 30% of patients for an SBP <180 mm Hg and in 75% for an SBP <200 mm Hg. The median time to follow-up BP check was 34 minutes (IQR 15-58). The median decrement in SBP was 20 mm Hg (IQR 5-37); however, the response to treatment was highly variable, with 2% of patients experiencing no change and 14% experiencing an increase in SBP. Seventy-nine patients (14%) had a decrement in SBP >25% following treatment.
Description of Quality Improvement Results
Following the QI initiative, a total of 934 patients experienced 9,743 episodes of asymptomatic elevated blood pressure over a 4-month period (November 1, 2017 to February 28, 2018). As shown in Table 1, patients in the postintervention period had a slightly higher median age (67 [IQR 55-80] vs 69 [IQR 57-83]; P = .01), a higher median APR-DRG weight (1.34 [IQR 0.99-1.77] vs 1.48 [1.00-1.82]; P < .001), and a longer median length of stay (4.6 [2.8-8.0] days vs 5.1 [2.9-9.2] days; P = .004). There was also a higher proportion of nonEnglish speakers, fewer Black patients, and a lower proportion of preexisting HTN, in the postintervention period.