Gap analysis: a strategy to improve the quality of care of head and neck cancer patients
Background Continuing assessment of cancer care delivery is paramount to the delivery of high-quality care. Head and neck cancer patients are vulnerable to flaws in care because of the complexity of medical and psychosocial conditions.
Objective To describe the use of a gap analysis and quality improvement interventions to maximize the coordination and care for patients with head and neck cancer.
Methods The gap analysis was comprised of a thorough literature review to determine best practice in the management of head and neck cancer patients and data collection on the care provided at a cancer center. Data collection methods included a clinician survey, a process map, and a patient satisfaction survey, and baseline data from 2013. A SWOT (strengths, weaknesses, opportunities, threats) analysis was conducted, followed with quality improvement interventions. A re-evaluation of key data points was conducted in 2015.
Results Through the clinician survey (n =25 respondents) gaps in care were identified and included insufficient preoperative education, inefficient discharge planning, and delayed dental consultations. The patient satisfaction survey indicated overall satisfaction with the care received at the cancer center. The process mapping (n =33 respondents) identified that the intervals between treatments did not always meet the best practice standards. The re-assessment revealed improvement with the process for nonsurgical patients by meeting the benchmark.The surgical cases revealed the interval between surgery and initiation of treatment was greatly improved, although it did not yet meet the benchmark.
Limitations Small sample size
Conclusions A gap analysis provides the structure to evaluate and improve cancer care services for head and neck cancer patients.
Accepted for publication January 9, 2017. Correspondence Mary Pat Lynch, MSN, CRNP, AOCNP; LynchMP@pahosp.com. Disclosures The authors report no disclosures or conflicts of interest.
JCSO 2017;15(1):28-36. ©2017 Frontline Medical Communications.
doi: https://doi.org/10.12788/jcso.0324.
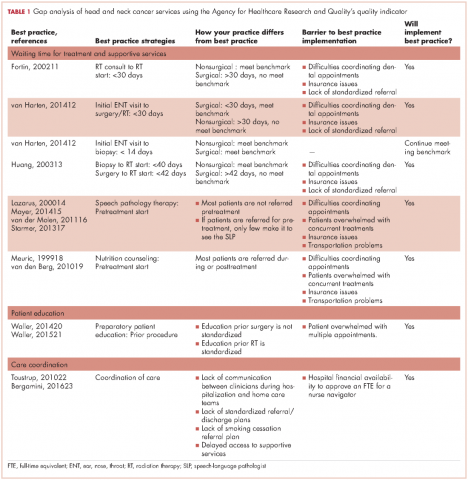
Measure gaps against benchmarks. To Gap analysis of measure gaps against benchmarks, the authors used the Agency for Health Care Research and Quality tool that provides a systematic method to compare current practice with best practices and determine the barriers to best practice and the feasibility of implementing best practices by the institution23 (Table 1). For this project, a process map of waiting time to treatment and supportive care interventions was created, so that real-world conditions could be measured against benchmarks.
Process map. The authors identified 67 newly diagnosed HNC patients during January-July 2014 from the surgery, radiation therapy, and nutrition departments, but only 33 patients were able to be tracked from their initial visit at the cancer center until the completion of their treatment through the electronic medical record (EMR) system. Their information was compiled in a spreadsheet based on the EMR information. Data included patient access to supportive services and number of days between important treatment benchmarks. Tracking data was used to create a treatment flow chart and determine average treatment intervals.
,To map the typical patient process, the patients were split into two groups: surgical (n = 22) and nonsurgical (n = 11). Surgical patients underwent surgery as their primary treatment and received adjuvant radiation therapy or concurrent chemotherapy. Nonsurgical patients did not require surgery other than biopsy as a part of their treatment. Most of the nonsurgical patients received chemotherapy, and 1 patient received palliative radiation therapy.
SWOT analysis. The SWOT analysis is used to chart institution performance in relation to benchmarks while describing stakeholders’ perceptions.24The stakeholder perspective for this project focused on the views of the health care providers from all disciplines regarding the quality of care provided to the HNC population. In addition, a patient survey was conducted to assess their perception of the care they received.
Clinician survey. We surveyed 25 clinicians, including physicians, advanced practice providers, nurses, and allied health professionals, from the surgical (n = 3), hospitalization (n = 6), radiation (n = 3), chemotherapy (n = 3) and supportive services teams (n = 10). The survey was conducted face to face and included 7 open-ended questions designed to gain insight about problems encountered with coordination of care, suggestions to improve coordination of care, factors in treatment delays, suggestions to decrease treatment delays, factors in excellent patient outcomes, rate overall patient care, and suggestions for improvement of service. Initial survey responses were filtered by recurring themes in each question among the different patient service teams.
Patient satisfaction survey. The sample of patients was obtained from the surgery, radiation therapy, and nutrition departments during January-July 2014. Sixty-seven initial patients were identified but only 43 were eligible for interview because they had a listed phone number. A six-question nonvalidated survey was developed by the authors to measure patient satisfaction with the scheduling process, waiting time, information provided about treatment and their medical status, emotional support, the coordination of care, and the payment process. Satisfaction was rated on a scale from 1 to 5 (1 = Poor, 2 = Fair, 3 = Satisfactory, 5 = Great).
Analysis and final report. See Results section.
Quality improvement implementation. The transitions and the education committees were created to address the gaps identified during the analysis. The transitions committee developed strategies to improve the coordination of care of HNC patients throughout their cancer treatment and the education committee elaborated new ways to enhance patient education while meeting treatment timeline standards. The implementation of the interventions was developed by the inpatient and outpatient MTD teams caring for the HNC population.
Re-assessment of indicators. During January-December 2015, a total of 58 patients diagnosed with HNC were identified. Of those, 40 patients with recurrent disease were eliminated, leaving 18 patients (10 surgical, 8 nonsurgical). Similar to the initial assessment for the gap analysis, data included patient access to supportive services and number of days between important treatment benchmarks. Tracking data was used to create a treatment flow chart and determine average treatment intervals.
Results
Most of the patients were men (70%), white (70%), and 60% were within the 50-69 years age range at the time of diagnosis.
Clinician survey
The clinicians were surveyed and their responses analyzed by two people, the project leader and the project assistant. The most commonly identified weaknesses in care that the clinicians identified were delayed access to dental referrals, insufficient preoperative patient education, and inefficient discharge planning and/or home care coordination. Dental referrals were identified as a major cause of delay in starting radiation therapy because of scheduling issues, a lack of patient motivation, limited insurance coverage, and difficulty identifying reliable dentists in the patient’s geographic area. Clinicians also identified problems coordinating smoking cessation referrals for patients.