Prevention of Type 2 Diabetes: Evidence and Strategies
Lifestyle Modifications
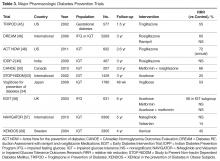
The alarming rapid increase in the prevalence of T2DM has been linked to a parallel rising epidemic of overweight, obesity, and lack of physical activity. Therefore, lifestyle changes aiming at weight reduction seemed to be a natural individual and public health strategy to prevent diabetes, and such strategies have been the focus of many randomized controlled trials around the world. As anticipated, weight loss, exercise, and diet have all been shown, separately or in combination, to be effective in decreasing the incidence of T2DM in high-risk patients [22–27]. Furthermore, and well beyond the benefit observed during the trials, follow-up studies revealed a sustained reduction of diabetes incidence in intervention groups several years after cessation of the intervention [28–32] (Table 2).
The Da Quing Diabetes Prevention Study (DQDPS), published in 1997, is one of the earliest prospective diabetes prevention trials [22]. This 6-year study conducted in 33 clinics in China from 1986 through 1992 included 577 participants with IGT who were randomly assigned to 1 of 4 groups: (1) diet (high vegetables, low sugar/alcohol) only, (2) exercise, (3) diet plus exercise, and (4) standard of care. At 6 years, diabetes incidence was significantly reduced by 46% in the exercise group, 31% in the diet group, and 42% in the diet plus exercise group compared to standard care. In 2006, 14 years after the end of the trial and 20 years after the initial enrollment, the cumulative incidence of diabetes was significantly lower in the intervention group at 80%, compared to 93% in the control group, and the annual incidence of diabetes was 7% and 11%, respectively, with a 43% lower incidence of diabetes over the 20-year period in the combination lifestyle changes group [28]. The preventive benefit of lifestyle changes persisted 2 decades after the initial randomization despite the standardization of treatment for all groups over the 14 years following the study, suggesting a strong and longitudinal preventive effect of the initial lifestyle modifications. In a follow-up study of the DQDPS conducted in 2009, at 23 years of follow-up, the cumulative incidences of cardiovascular mortality and all-cause mortality were significantly lower in the intervention group (11.9% versus 19.6%, and 28.1% versus 38.4%, respectively), highlighting the long-term clinical benefits of lifestyle intervention in patients with IGT [29].
Similarly, the Finnish Diabetes Prevention Study (FDPS), published in 2001, enrolled 522 middle-aged overweight participants with IGT [23]. The participants randomly assigned to the intervention group received individualized counseling designed to reduce weight, decrease total intake of fat and saturated fat, increase intake of fiber, and increase physical activity. The control group received standard therapy. At 4 years of follow-up, the cumulative incidence of diabetes was 11% in the intervention group and 23% in the control group, with a statistically significant 58% reduction in risk for progression to diabetes. A follow-up of the FDPS was published in 2006 [31]. Participants who did not progress to diabetes in the initial 4-year study were further followed for a median of 3 years. Interestingly, lifestyle changes were maintained by the intervention group participants despite the cessation of the individual counseling, leading to a 36% relative reduction in diabetes incidence during the post-intervention follow-up period alone (4.6 vs 7.2 per 100 person-years, P = 0.041) and a 43% cumulative diabetes incidence reduction over the 7-year follow-up, demonstrating, one more time, the sustained efficacy of lifestyle changes.
In the United States, the Diabetes Prevention Program (DPP) trial is a landmark NIH-sponsored multicenter randomized controlled trial published in 2002, and one of the largest diabetes prevention studies with lifestyle changes to date [24]. A total of 3234 participants with prediabetes, defined as an IFG or IGT, were randomly assigned to an intensive lifestyle modification program, metformin 850 mg twice daily, or matching placebo. Lifestyle changes included a low-fat (< 25% of caloric intake), 1200- to 1800-calorie diet and exercise for 150 minutes a week, with a 7% body weight reduction goal and a very well structured curriculum and professional support group. The study was discontinued early (at 3 years) as the data demonstrated the superiority of lifestyle changes, with a 58% reduction in diabetes incidence in the lifestyle intervention group and a 31% reduction in the metformin group when compared to placebo (cumulative incidence of diabetes at 3 years of 28.9%, 21.7 %, and 14.4% in the placebo, metformin, and lifestyle intervention groups, respectively). Lifestyle changes were significantly more effective than metformin and were consistently effective in men and women across age, BMI, and ethnic groups.
The DPPOS (DPP Outcome Study) was a 10-year follow-up of the DPP study published in 2009 where all participants were offered group-implemented lifestyle changes and were followed for an additional 5.7 years [32]. Unlike the Finnish follow-up study, diabetes incidence was similar in the 3 treatment groups in the follow-up period. However, the cumulative incidence of diabetes remained significantly the lowest in the original lifestyle group, with a 34% cumulative risk reduction in the lifestyle group and an 18% reduction in the metformin group at 10 years when compared to placebo. Interestingly, unlike most other studies of weight-reducing interventions, in the DPPOS, patients in the lifestyle changes and metformin groups maintained weight loss at 10 years’ follow-up.
In Japan, a diabetes prevention study assigned 458 male participants with IGT to a standard intervention group or an intensive intervention group receiving detailed lifestyle modification counseling every 3 to 4 months during hospital visits [25]. The cumulative 4-year incidence of diabetes was 9.3% in the control group versus 3.0% in the intervention group, and the reduction in diabetes risk was 67.4% (P < 0.001), with body weight reductions of 0.39 kg and 2.18 kg, respectively (P < 0.001). Of note, participants with higher FBG at baseline developed diabetes at a higher rate than those with lower values. This study suggested that lifestyle change counseling conducted in an outpatient clinic setting can be very effective in preventing diabetes.
Indian adults are thought to be more insulin resistant at a younger age and at a lower BMI than Caucasians. To assess whether the DPP findings can be replicated in an Indian population, the Indian Diabetes Prevention Program (IDPP) trial randomized a total of 531 participants with IGT to 4 groups: control, lifestyle modification, metformin, and lifestyle modifications with metformin [26]. The 3-year cumulative incidences of diabetes were 55.0%, 39.3%, 40.5%, and 39.5%, respectively, showing again a significant relative reduction in progression to diabetes of 28.5% with lifestyle changes, 26.4% with metformin, and 28.2% with both lifestyle changes and metformin, as compared with the control group.
In a Japanese unmasked, multicenter, randomized controlled trial published in 2011, 641 overweight adults with IFG were randomized to a frequent intervention group, receiving individual counseling and support for lifestyle modifications 9 times over 36 months, or a control group, receiving counseling 4 times over the same period. The 3-year cumulative incidence of T2DM was significantly lower in the frequent intervention group than in the control group (12.2% vs 16.6%) [27]. Interestingly, in a posthoc subgroup analysis, the protective effect was more prominent in patients with underlying associated IGT or elevated A1C, but was not observed in patients with isolated IFG, suggesting a possible prognostic value of an additional A1C or oral glucose tolerance test in individuals with IFG.