Making Quality Real for Physicians
Maintenance of Certification
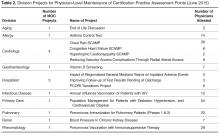
As of 2013, physicians who were board certified by the ABIM or ABMS were required to attain 20 practice assessment points showing participation in quality improvement activities for maintenance of certification (MOC). Although ABIM suspended the practice assessment requirement in 2015, it is likely that some component of quality improvement will be assessed in the future [5,19]. Prior to the changes in 2015, we were approached by the hospital leadership to roll out a new, streamlined process to leverage our existing quality metrics and established performance improvement plans in order to allow physicians to gain MOC credit. Each metric/project was vetted with 3 separate groups: the DOMQP, hospital leadership leading the MOC efforts, and Partners Healthcare, our overarching local health care system. We worked with our division physician champions and the physicians preparing for board re-certification to complete the one-time documentation required by the hospital for MOC. This process took approximately 6 months per project. Once the project was approved by all 3 channels, all physicians participating in the quality effort could get the practice assessment points by completing a simple attestation form.
Current Focus
After the stabilization of our new EHR and the re-creation of former reports, the program began to engage divisions in new measures. We still focus on chronic disease management and vaccinations but instead try to create a unified approach across multiple divisions within the DOM. Building upon our previous work in the renal division, over the past year we convened a hyper-tension work group comprising physician leads from endocrine, cardiology, renal, primary care, gerontology, neurology, pharmacy, and obstetrics. The goal of these meetings is to optimize blood pressure management across different patient populations by creating a centralized hospital approach with an algorithm agreed upon by the physician workgroup. We were able to secure additional internal grant funding to develop a pilot project where bluetooth blood pressure cuffs are given to eligible hypertensive patients in our pilot ambulatory practices. The daily blood pressure readings are transmitted into the EHR and a nurse practitioner or pharmacist contacts the patient at defined intervals to address any barriers and titrate medications as necessary. Analysis of the outcomes will be presented this fall. Similarly with vaccinations we are creating an automated order form within the EHR that will appear whenever a specialist places an order to start immunosuppressive medications. This will prompt the provider to order appropriate labs and vaccinations recommended for the course of treatment.
In addition to expanding upon previous metrics, we have expanded our scope to focus on patient safety measures, specifically, missed and delayed cancer diagnoses of the lung and colon. We are working on processes to track every patient with an abnormal finding from point of notification to completion of recommended follow-up at the appropriate intervals. Also we have now have 3 projects in the inpatient setting: chronic obstructive pulmonary disease (COPD) readmissions, and 2 standardized clinical assessment and management pathways (SCAMPs), one on acute kidney injury and the other on congestive heart failure [20]. The COPD project aims to have every patient admitted with COPD receive a pulmonary and respiratory consult during their stay and a follow-up visit with a pulmonologist. The goal of any SCAMP is to standardize care in an area where there is a lot of variability through the use of clinical pathways.
Communication Strategy
In order for the DOMQP to ensure that multiple quality requirements are met by all divisions, we have established a robust communication strategy with the goal of clear, concise, and relevant information-sharing with physicians and staff. We engage physicians through direct meetings, regular emails, and data reporting. The purpose of our outreach to the division faculty is threefold: (1) to educate physicians about hospital-wide programs, (2) to orient them to specific action items required for success, and (3) to funnel questions back to project leaders to ensure that the feedback of clinicians was incorporated into hospital wide quality initiatives. Our first challenge is to provide context for physicians about the project, be it based on accreditation, credentialing or a federal mandate. We work with the hospital project leaders to learn as much as possible about the efforts they are promoting so we can work in concert with them to highlight key messages to physicians.
Next, we establish a schedule to present at each clinical specialty faculty meeting on a regular basis (semi-annually to quarterly). At these meetings we present an overall picture of the key initiatives relevant to the division, identify milestones, offer clear timelines and prioritization of these projects, and narrow the focus of work to a few bulleted action items for all levels of the clinic staff to incorporate into its workflow. We then listen to questions and concerns and bring these back to the initiative leaders so that systematic changes can be made. Answers and updates are communicated back to the divisions, thus closing the communication loop. We interface with practice managers and clinical support staff to identify opportunities for them to support physicians in meeting initiative requirements [21,22].
In addition to presenting at faculty meetings, we present updates to departmental and hospital leadership, including vice chairs and division chiefs. These meetings include high-level data on performance as well as an opportunity to discuss the challenges we identified through our discussions with individual specialties. These forums are a good place to discuss overarching process issues or to disseminate answers to previous questions.
An important part of our communication plan involves our comprehensive monthly emails. For each initiative, we receive department level data on a monthly basis from the project leadership. We deconstruct these reports to enable us to evaluate our 13 divisions individually. We show performance at the physician level and highlight general areas where improvement is needed. We send monthly e-mails to division clinical and administrative leadership to apprise them of their division’s performance and inform them of areas that require concentrated effort. Depending on the initiative, we present data as a snapshot in time or trend over time. From 2012–2017 the DOMQP has helped to bridge the gap between large-scale rollouts of the new initiatives and the vast number of DOM physicians who required more specific education and tools to meet these new requirements.