Making Quality Real for Physicians
Meaningful Use
Our team was responsible for ensuring that the DOM succeeded in the federal government’s MU program. Millions of dollars were at risk to the hospital and to physicians based on performance on various MU metrics. The hospital made this a priority and set a goal for 90% of eligible providers to successfully certify in Stage 1 as meaningful users in the first year of MU.
While working with the clinics to achieve meaningful use, we recognized that a range of staff members played a critical role in helping physicians meet MU metric targets. We worked with the clinic and departmental administrative leadership to set up a one-time bonus payment in 2013 to all DOM clinic staff, including medical assistants, licensed practical nurses, practice assistants, for appreciation of their significant efforts to help the physicians and the hospital achieve their MU goals. As health care delivery continues to rely more heavily on highly functional teams, acknowledgment of the efforts of non-clinical staff in helping front-line clinicians in achieving MU can help promote teamwork around a common goal.
Our partnership with the hospital MU team lead to a final tally of 98% of eligible providers meeting stage 1 in 2013, 99% in 2014 and 100% for the modified stage 2 in 2015 and 99% in 2016 for DOM specialty divisions, representing over 250 physicians.
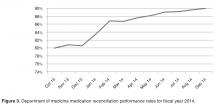
Medication Reconciliation
The impetus for the hospital’s focus on medication reconciliation was the Joint Commission requirement that medications listed as prescribed in the EHR be reconciled with the patient at each visit [10]. The hospital’s quality and safety team created a hospital-wide metric aligned with hospital policy to measure how providers were reconciling medication lists during office visits. The medication reconciliation metric tallied visits when a medication change occurred (denominator) in which all of the medications originally prescribed by a physician in that specialty clinic were reconciled (numerator). This made it easier for specialists to buy-in to the metric because they were only responsible for the medications they prescribed and not the entire list. To meet the metric, physicians are required to take an action on each of the medications they prescribed by clicking taking, not taking, taking differently, or discontinuing. If the clinic has additional staff within the clinic to assist in the medication review process with the patient, physicians would receive credit for their actions once they had reviewed the medication list.
The metric BWH established to measure medication reconciliation was distinct and more rigorous than the medication reconciliation metric used to meet MU requirements. This presented a challenge in both physician communication regarding requirements and data sharing to drive performance improvement. Since the DOM is the largest and most prescribing department, we had to work with clinical and administrative leaders at the divisional level so that all staff understood the exact requirements and how to achieve them. When presenting to faculty we encountered many questions, and general resistance to more clicks in the EHR, as there was no universal “reconcile” button in the extant EHR. After breaking down the process into discrete components with staff and analyzing the data, we targeted outreach to the specific divisions and clinics that needed additional education and support. In our monthly email communication to division leadership, we displayed comparative data on all divisions within the DOM.
After we transitioned to a new vendor-based EHR in 2015, we developed a new medication reconciliation metric, aimed to align with Stage 2 MU requirements, and ensured all divisions had processes in place to review and reconcile medications. In our new EHR, medications lists are shared and viewable between ambulatory and inpatient environments and discharge summaries contain changes made to medications while inpatient. We have found that our performance on our new metric is 70.5% for February 2017 and we are continuing to educate physicians and staff on our new EHR functionality, our new electronic measurement and on workflows to help assist with improving performance with a short-term goal of 80%. We have found that our new EHR functionality does not match the ease of our old EHR functionality, which has made improvement on this metric a significant challenge for our clinicians and staff.