Annular plaques on the back and flanks
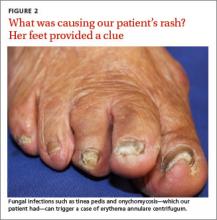
The combination of a ring-shaped rash on the patient’s torso and a foot infection led us to the diagnosis.
Diagnosis: Erythema annulare centrifugum
Potassium hydroxide (KOH) testing and culture of the rash were negative, but a KOH of the skin between her toes and her toenails revealed septate hyphae, which confirmed a diagnosis of tinea pedis and onychomycosis. The combination of tinea pedis/onychomycosis and the clinical appearance of the rash on the patient’s flanks led us to diagnose erythema annulare centrifugum (EAC) in this patient.
EAC is a noninfectious hypersensitivity phenomenon.1 It is most commonly associated with dermatophyte fungi, but other inciting agents include candida, penicillium in blue cheese, viruses (varicella zoster virus, human immunodeficiency virus, Epstein-Barr virus), ectoparasites (phthirus pubis), and, rarely, certain medications, including diuretics, finasteride, nonsteroidal anti-inflammatory drugs, antimalarials, and amitriptyline.2-6 Hormonal changes during pregnancy and neoplasms have occasionally been associated with EAC.2-4
Histologic findings are nonspecific in EAC, but a biopsy may be performed to exclude other conditions. Superficial EAC demonstrates histologic changes primarily in the epidermis, including spongiosis, parakeratosis, and a superficial inflammatory infiltrate.8 The deep variant demonstrates superficial to deep dermal lymphocytic inflammatory infiltrate in a perivascular “sleeve-like” distribution with little epidermal change.7,8
Differential diagnosis includes figurate erythemas
The differential diagnosis includes figurate erythemas (erythema chronicum migrans and erythema marginatum) and other conditions with annular, scaling plaques (tinea corporis [ringworm], annular psoriasis, pityriasis rosea, syphilis (secondary stage), and mycosis fungoides).2,9
Figurate erythemas. Unlike EAC, figurate erythemas are non-scaling annular lesions. Erythema chronicum migrans is a manifestation of Lyme disease. It is characterized by papules that expand peripherally at the site of a tick bite. In some cases, secondary lesions distant from the bite occur. Erythema marginatum is associated with rheumatic fever. These nonpruritic red circular rings without scale are unique in their capacity to expand several centimeters per day.
Conditions characterized by annular scaling plaques. Tinea corporis presents as round red patches that slowly become ring-shaped, with a raised border and clear center. Unlike EAC, the scale is present at the leading border of the rings.