Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: A randomized controlled trial
Experimental subjects spent fewer 2-week blocks with nasal congestion, sinus headache, and frontal pain and pressure and used antibiotics and nasal sprays in fewer blocks (Table 3).
Forty-four experimental subjects answered questions about satisfaction and side effects. Forty-two stated they “will continue to use” nasal irrigation; the remaining 2 subjects found nasal irrigation less helpful but did not experience side effects. All 44 subjects “would recommend” nasal irrigation to friends or family with sinus problems. Ten subjects (23%) experienced side effects; 8 identified nasal irritation, nasal burning, tearing, nosebleeds, headache, or nasal drainage as occurring but “not significant.” Two subjects identified nasal burning, irritation, and headache as “significant,” but this did not change their high satisfaction rating. Of the 10 subjects who experienced side effects, 4 reduced or eliminated the side effects by temporarily alternating treatment days or decreasing salinity by 50%.
TABLE 2
Primary outcomes: RSDI, SF-12, and SIA baseline scores and mean score changes*
| Status | Baseline score | Baseline vs score change at | ||
|---|---|---|---|---|
| 1.5 mo | 3 mo | 6 mo | ||
| RSDI | ||||
| Experimental | 58.4 ± 2.0 | 8.2 ± 1.2 | 14.0 ± 2.0† | 14.4 ± 1.7‡ |
| Control | 59.6 ± 3.0 | 5.6 ± 1.4 | 7.7 ± 1.9 | 0.9 ± 1.0 |
| SF-12 | ||||
| Experimental | 60.3 ± 3.0 | 6.7 ± 2.1 | 8.2 ± 2.9 | 12.7 ± 3.6 |
| Control | 59.3 ± 3.9 | 5.4 ± 3.9 | 2.9 ± 4.0 | 2.2 ± 3.5 |
| SIA | ||||
| Experimental | 3.9 ± 0.1 | -0.8 ± 0.2† | -1.2 ± 0.2† | -1.6 ± 0.2‡ |
| Control | 4.1 ± 0.2 | -0.02 ± 0.21 | -0.3 ± 0.2 | -0.005 ± 0.2 |
| *Data are presented as mean ± standard error. | ||||
| †Statistically significant at P < .05. | ||||
| ‡Statistically significant at P < .001. | ||||
| RSDI, Rhinosinusitis Disability Index; SF-12, Medical Outcomes Survey Short Form 12; SIA, Single-Item Symptom Severity Assessment. | ||||
TABLE 3
Secondary outcomes
| Secondary outcome | Experimental | Control |
|---|---|---|
| Sinus symptoms* | ||
| Sinus headache† | 57 ± 0.05 | 76 ± 0.06 |
| Frontal pain‡ | 55 ± 0.05 | 82 ± 0.05 |
| Frontal pressure‡ | 53 ± 0.05 | 86 ± 0.05 |
| Nasal congestion† | 67 ± 0.04 | 83 ± 0.05 |
| Nasal discharge | 65 ± 0.05 | 69 ± 0.07 |
| Medication use* | ||
| Antibiotics† | 10 ± 0.02 | 19 ± 0.04 |
| Nasal sprays§ | 4 ± 0.01 | 8 ± 0.02 |
| EQ: sinus symptoms related to QOL|| | ||
| Better‡ | 41 (93) | 2 (9) |
| Same‡ | 3 (7) | 16 (73) |
| Worse‡ | 0 (0) | 4 (18) |
| *Data are presented as the percentage of 2-week blocks ± standard error during the study. | ||
| †Statistically significant difference between groups: P < .05. | ||
| ‡Statistically significant difference between groups: P < .001. | ||
| §Not statistically significant, difference between groups: P = .06. | ||
| || Data are presented as number (%) of subjects. | ||
| EQ, exit questionnaire (Is your quality of life with respect to sinus symptoms better or worse since the beginning of the study?); QOL, quality of life. | ||
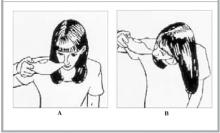
FIGURE 1
Position of nasal cup for nasal irrigation therapy A B
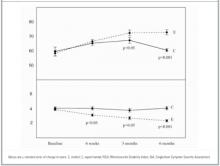
FIGURE 2
Mean RSDI and SIA scores in control and experimental subjects
DISCUSSION
Our trial of daily hypertonic nasal irrigation produced several significant findings. We found consistent, statistically significant improvements in QOL (RSDI) and overall symptom severity (SIA). This was consistent with QOL improvement previously reported over short periods with the use of disease-specific measures.12-14 The RSDI is a moderately well-developed and validated disease-specific QOL instrument.21-23 The “minimal clinically important difference,” defined as the average score improvement needed to justify costs and risks,24-26 has not been established for sinusitis. However, it has been estimated for other disease states. For example, a half-point change on a 7-point Likert scale corresponds to estimates of important change in patients with chronic heart and lung disease.22,27 Others have found similar relationships.28-31 In our study, RSDI scores among treated subjects averaged 6.0 and 15.5 points better than controls at 3 and 6 months, respectively. On the SIA, treated subjects averaged 0.6, 0.9, and 1.6 points better. Extrapolating from these findings, these differences appear to be clinically significant. By using 10% improvement of the RSDI, our data showed numbers needed to treat of 9, 5, and 2 at 1.5, 3, and 6 months, respectively (95% confidence interval at 6 months, 1.4–2.6). Numbers needed to treat for SIA, symptom frequency, and medication use were similar. SF-12 improvement, although not statistically significant in this small trial, may represent clinically significant improvements in general health-related QOL.
“Percentage change” is used often by clinicians to gauge therapeutic progress. Ours is the first study to document such change in sinusitis patients using nasal irrigation. Ours is also the first trial to show decreased symptom frequency over a 6-month period. Shorter trials have documented improvement in patients with nasal symptoms12,13,17,18 or with chronic sinusitis in adult14,15 and pediatric16 populations. Consistent with improved symptoms and QOL, experimental subjects decreased their use of antibiotics and nasal sprays, as previously reported in a short trial.12
Side effects have not been carefully assessed in previous trials. Although generally safe, daily hypertonic nasal irrigation was associated with some clinically minor side effects. Interestingly, subjects were able to decrease side effects by adjusting irrigation schedule or salinity. Side effects were not sufficiently bothersome to stop therapy. Compliance with daily therapy was very high and is previously unreported. Although this was consistent with a positive effect on relatively severe symptoms, we believe high compliance also was related to teaching, demonstrated proficiency with nasal irrigation, and close telephone follow-up. One prior study reported subjects’ observation of the first nasal irrigation15; several studies reported providing some education.1214,18