Autonomic dysfunction: A guide for FPs
Impotence, bladder dysfunction, GI symptoms, and orthostatic hypotension can signal autonomic dysfunction. Here’s what you’ll see and how to respond.
PRACTICE RECOMMENDATIONS
› Begin a trial of an antimuscarinic if initial nonpharmacologic treatment of urge incontinence or overactive bladder is ineffective. B
› Start step-wise treatment beginning with metoclopramide A, followed by domperidone, and, finally, oral erythromycin B in patients with gastroparesis who have failed conservative measures.
› Employ step-wise pharmacologic treatment, starting with fludrocortisone, for patients with disabling symptoms of orthostatic hypotension who fail to respond to nonpharmacologic measures. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
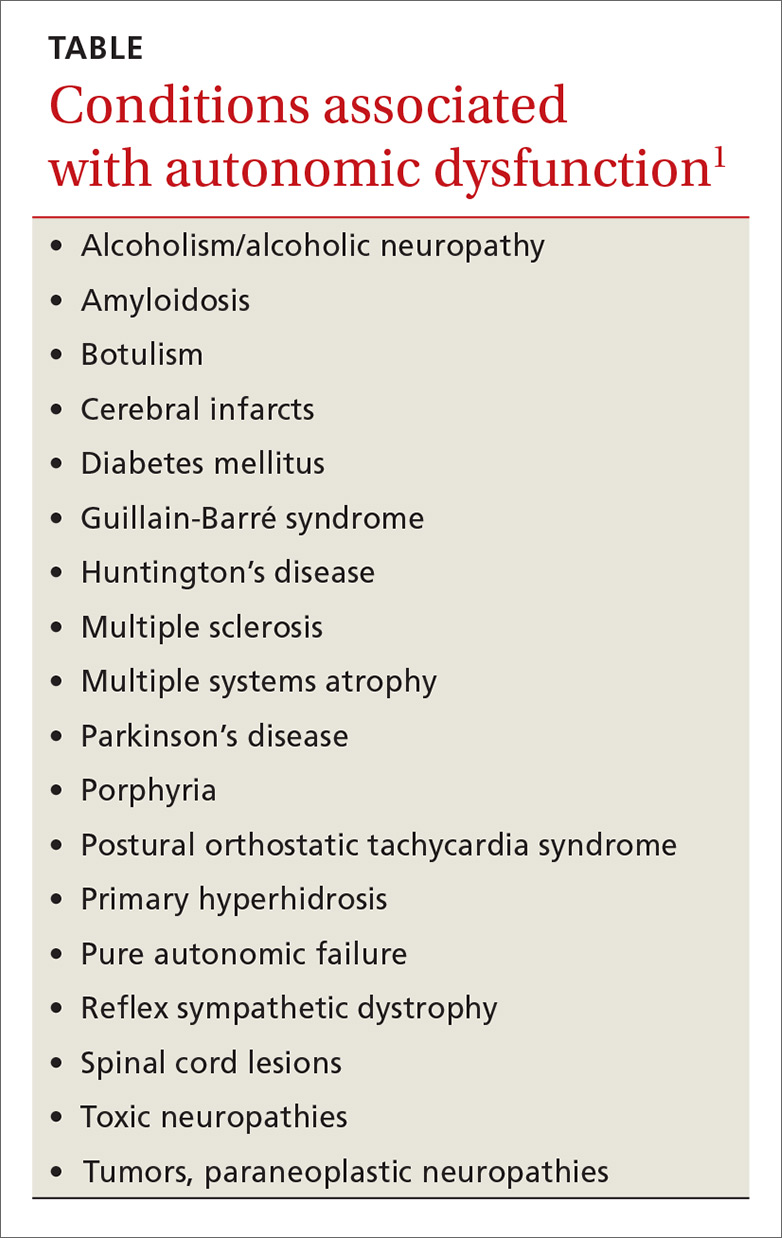
Signs and symptoms of autonomic dysfunction commonly present in the primary care setting. Potential causes of dysfunction include certain medications and age-related changes in physiology, as well as conditions such as diabetes mellitus, multiple sclerosis, and Parkinson’s disease (TABLE1). This evidence-based review details common manifestations of autonomic dysfunction, provides a streamlined approach to patients presenting with symptoms, and reviews appropriate step-wise management.
When a delicate balance is disrupted
The autonomic nervous system provides brisk physiologic adjustments necessary to maintain homeostasis. Physiologic functions impacted by the central nervous system include: heart rate, blood pressure (BP), tone of the bladder sphincter and detrusor muscle, bowel motility, bronchodilation and constriction, pupillary dilation and constriction, sweating, catecholamine release, erection, ejaculation and orgasm, tearing, and salivation.1
Disorders of the autonomic system may result from pathologies of the central or peripheral nervous system or from medications including some antihypertensives, selective serotonin-reuptake inhibitors (SSRIs), and opioids.1 Such disorders tend to be grouped into one of 3 categories: those involving the brain, those involving the spinal cord, and autonomic neuropathies.1
The source of dysautonomia can often be determined by clinical context, coexisting neurologic abnormalities, targeted testing of the autonomic nervous system, and neuroimaging.1
Worrisome symptoms prompt a visit
A thorough history is critical to zeroing in on a patient’s complaints and ultimately providing treatment that will help manage symptoms.
When patient complaints are suggestive of autonomic dysfunction, a review of systems should include inquiry about lightheadedness, abnormal salivation, temperature changes of the extremities, gastrointestinal issues (vomiting, constipation, or diarrhea), and symptoms of presyncope/syncope or urinary or sexual dysfunction.1 The physical exam should include recordings of BP and heart rate in the supine and standing positions and a complete neurologic examination.1 Findings will typically point to one or more common complications.
Common complications of autonomic dysfunction
Complications of autonomic dysfunction include impotence, bladder dysfunction, gastrointestinal (GI) dysfunction, and orthostatic hypotension and vasomotor abnormalities. A less common condition—autonomic dysreflexia, which is a distinct type of autonomic dysfunction, and a true medical emergency—is also important to keep in mind.
Impotence
Autonomic neuropathy is a common cause of impotence and retrograde ejaculation. Loss of early morning erections and complete loss of nocturnal erections often have an etiology related to vascular disease and/or autonomic neuropathy. In addition, poor glycemic control and vascular risk factors appear to be associated with the development of diabetic autonomic neuropathy.2
Development of an erection requires an increase in parasympathetic activity and a decrease in sympathetic output. Nocturnal penile tumescence testing has been used to infer parasympathetic damage to the penis in men with diabetes who do not have vascular disease.3
First- and second-line agents. Phosphodiesterase-5 inhibitors (eg, sildenafil, tadalafil, vardenafil) have demonstrated efficacy in improving the ability to achieve and maintain erections in patients with autonomic dysfunction, including diabetic autonomic neuropathy.4-6 Second-line therapies with proven efficacy include intraurethral application and intracavernosal injections of alprostadil.7,8
Bladder dysfunction
Sympathetic activity increases bladder sphincter tone and inhibits detrusor activity, while the parasympathetic nervous system increases detrusor activity and decreases sphincter tone to aid in voiding.1 Disrupted autonomic activity can lead to urinary frequency, retention, and hesitancy; overactive bladder; and incontinence.1 Brain and spinal cord disease above the level of the lumbar spine results in urinary frequency and small bladder volumes, whereas diseases involving autonomic nerve fibers to and from the bladder result in large bladder volumes and overflow incontinence.9
Patients presenting with lower urinary tract symptoms require a comprehensive evaluation to rule out other pathologies, as the differential for such symptoms is broad and includes infection, malignancies, interstitial cystitis, and bladder stones. The initial evaluation of lower urinary tract symptoms should include a history and physical exam including that of the abdomen, pelvis, and neurologic system. Lab work should assess renal function and blood glucose, and should include urinalysis and culture to rule out infection and/or hematuria. A prostate-specific antigen (PSA) test may be appropriate in men with a life expectancy >10 years, after counseling regarding the risks and benefits of screening.
Anticholinergic drugs with antimuscarinic effects, such as oxybutynin, may be used to treat symptoms of urge incontinence and overactive bladder. They work to suppress involuntary contractions of the bladder’s smooth muscle by blocking the release of acetylcholine. These medications relax the bladder’s outer layer of muscle—the detrusor. Such medications often have a number of anticholinergic adverse effects, such as dry mouth and constipation, sometimes leading to discontinuation. A post-void residual (PVR) test may be helpful in guiding management. For example, caution should be used in patients with elevated PVRs, as anticholinergics can worsen urinary retention.
Beta-3 agonists (eg, mirabegron) are a novel class of medications used to treat overactive bladder. These medications act to increase sympathetic tone in the bladder. Because they have the potential to raise BP, monitor BP in patients taking these agents. In addition, monitor patients taking antimuscarinics or beta-3 agonists for the development of urinary retention.
Other tests, treatments. Urodynamic testing is recommended for patients who fail to respond to treatment. Combining behavioral therapy with medication has been shown to be effective in patients with urge incontinence.10 Botulinum toxin type A, injected directly into the detrusor muscle, can be as effective as medication in patients with urinary urge incontinence.11
Detrusor underactivity is defined as contraction of reduced strength and/or duration, resulting in prolonged bladder emptying and/or a failure to achieve complete bladder emptying within a normal timespan.12 This diagnosis is typically made using urodynamic testing.13 PVRs ≥150 mL are considered evidence of urinary retention. Overflow incontinence can result from detrusor underactivity.
Consider a trial of a cholinergic agonist, such as bethanechol, in patients with urinary retention. Some patients will require intermittent straight catheterization or chronic indwelling foley or suprapubic catheters to void.






