Acute Limb Arterial Ischemia
Treatment
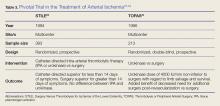
Definitive treatment decisions should be made in consultation with vascular surgery services. The results of three clinical trials developed the foundation for management of ALI: the Thrombolysis or Peripheral Arterial Surgery (TOPAS) trial, Surgery Versus Thrombolysis for Ischemia of the Lower Extremity (STILE) trial, and Rutherford trial.22-24 Table 3 provides a summary of the treatment techniques utilized, which include mechanical recanalization with percutaneous aspiration thrombectomy, percutaneous mechanical thrombectomy,6,12,25-28 pharmacological recanalization via catheter-directed thrombolysis,6,8,12,20,23-28 and/or surgical management via thrombectomy or embolectomy.6,11,23,24,27
Complications
The complications of treating ALI can be stratified into three subsets: pharmacologic, mechanical, and reperfusion injury-related. Medical treatment with heparin is not without risk. Intracranial hemorrhage, major bleeding at other sites, and compartment syndrome secondary to bleeding can all occur. Treatment may also cause distal embolization and lead to mechanical occlusion of another site. Finally, reperfusion injury predisposes the patient to a host of new problems. Reperfusion injury occurs when fresh blood enters a previously ischemic zone. When this occurs, oxygen free radicals, inflammatory mediators, and catabolism byproducts mix with the blood. This process can damage surrounding epithelial cells and lead to increased interstitial permeability. As a result, compartment syndrome may also develop via this mechanism.1,3,5,6 The anterior compartment of the lower extremity is most at risk. As such, assessment of peroneal nerve activity via dorsiflexion of the foot and sensation testing is important after the initiation of treatment.6 Systemic distribution of these harmful byproducts can also cause arrhythmias, renal failure, and systemic acadisos.1,3,5,6 It is important for physicians and staff to monitor the patient closely for the development of these complications and be prepared to intervene.
Opportunities for Improvement
In a condition where minutes matter, expedient action is critical. Time-to-recognition, imaging, consultation, and intervention all are potential sources of delay. Two recent studies have investigated the treatment timeline of ALI. The first study showed that the greatest source of delay is time from symptom onset to presentation in the ED; an average of 11.35 hours. The second largest source of delay was time from recognition of ALI to imaging, with an average delay of 4.75 hours. The average ED evaluation time was 40 minutes, and the average total time to intervention was 10.2 hours. While time-to-symptom presentation may represent a failure of public health, time-to-imaging was identified as an area of unacceptable delay by the authors.29 A second study examined the effect of pre-hospital care on the time-to-treatment. Persons who were transported via emergency medical services (EMS) arrived to the hospital at a median time of 5 hours after symptom onset, were seen by a physician at a median time of 51 minutes, and had revascularization at a median time of 23 hours. Those not transported by EMS arrived to the hospital at a median time of 48 hours after symptom onset, were seen by a physician at a median time of 80 minutes, and had revascularization at a median time of 93 hours. As a secondary goal, the study examined the effect of heparinization in the ED and showed that treatment with heparin was associated with a favorable outcome.30 While the total treatment times in each study vary widely, they share several important commonalities and reinforce expedient management as an important goal.
Outcomes
Advances in the treatment of this condition began in the 1970s, with an explosion of new techniques and data in the past several years. Still, ALI is a high morbidity and high mortality condition. Rates of limb loss are approximately 30% for all cases, and it is a fatal condition for as many as one-in-five. As discussed earlier, the patients who are most likely to experience ALI typically have several medical comorbidities. Perhaps unsurprisingly, ALI portends a poor prognosis even if the limb is salvaged. Approximately 15% to 20% of patients with ALI will die within 1 year of diagnosis.3,4,6,12
Conclusion
Acute limb ischemia is a rare condition, but a true medical emergency. Prompt recognition of the signs and symptoms of ALI are critical for optimizing patient outcomes. A high index of clinical suspicion in patients with risk factors may lead to early diagnosis. Early vascular surgery consultation and early IV heparin treatment are important aspects of care. Prompt imaging and staging guide further management. Special care should be paid to possible post-treatment complications and to the investigation of contributing factors. The EP has a great opportunity to positively impact care with expeditious management. Early diagnosis, targeted history and physical examination, prompt treatment, collaboration with specialists, and prevention and treatment of life-threatening complications are all hallmarks of emergency medicine.