Disease Burden and Quality of Life in Psoriasis Patients With and Without Comorbid Psoriatic Arthritis: Results From National Psoriasis Foundation Panel Surveys
The comorbidity profile and overall disease impact are not well understood in psoriasis with and without comorbid psoriatic arthritis (PsA). The objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related quality of life (QOL) in patients with moderate to severe psoriasis with and without comorbid PsA using results from National Psoriasis Foundation (NPF) surveys. The study included 3395 and 2072 patients with psoriasis alone and psoriasis with PsA, respectively. The results showed the burden of psoriasis either independently or with comorbid PsA. As severity of psoriasis increased, patient health and QOL were found to decline.
Practice Points
- Patients with psoriatic arthritis (PsA) often have severe cutaneous psoriasis. These patients may be at higher risk for comorbid conditions and impaired quality of life (QOL) compared to patients with psoriasis alone.
- The severity of cutaneous psoriasis, both in patients with psoriasis alone and those with comorbid PsA, is remarkable and is associated with worse QOL scores.
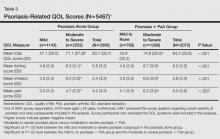
Psoriasis-Related QOL
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.