Idiopathic Granulomatous Mastitis
Idiopathic granulomatous mastitis (IGM) is a rare, poorly understood condition that presents as inflammatory nodules of the breast. It is often initially misdiagnosed as furunculosis or cellulitis. Despite the painful, scarring, and debilitating nature of the disease, patients often have a delay in accurate diagnosis and treatment. Even when IGM is considered as a diagnosis, it is one of exclusion, with the differential diagnosis including serious conditions such as breast cancer, sarcoidosis, and cutaneous tuberculosis. Therefore, appropriate workup is important. Given that IGM is a disease of the skin, it is important for dermatologists to be familiar with its presentation. We describe 3 cases of young women with this condition and demonstrate that identification of triggers or methotrexate treatment is highly successful in sparing patients the drastic surgical alternative of mastectomy.
Practice Points
- Idiopathic granulomatous mastitis (IGM) is a painful and scarring rare granulomatous breast disorder that can have a prolonged time to diagnosis that delays proper treatment.
- The pathogenesis of IGM remains poorly understood. The temporal association of the disorder with breastfeeding suggests that hyperprolactinemia or an immune response to local lobular secretions might play a role.
- Although many cases of IGM resolve without treatment, more severe cases can persist for a long period before adequate symptomatic treatment is provided with methotrexate, corticosteroids, or surgical excision.
- Before any of these therapies are applied, however, contributing factors, such as long-term breastfeeding and drugs that induce hyperprolactinemia, should be identified and withdrawn.
Patient 2
A 40-year-old woman with no history of breastfeeding who gave birth 4.5 years prior presented to her primary care provider with a painful breast lump and rash on the right breast of 2 months’ duration. Infectious mastitis was suspected; she was given cephalexin and clindamycin without improvement of symptoms.
Imaging
Mammography and ultrasonography were nondiagnostic.
Biopsy
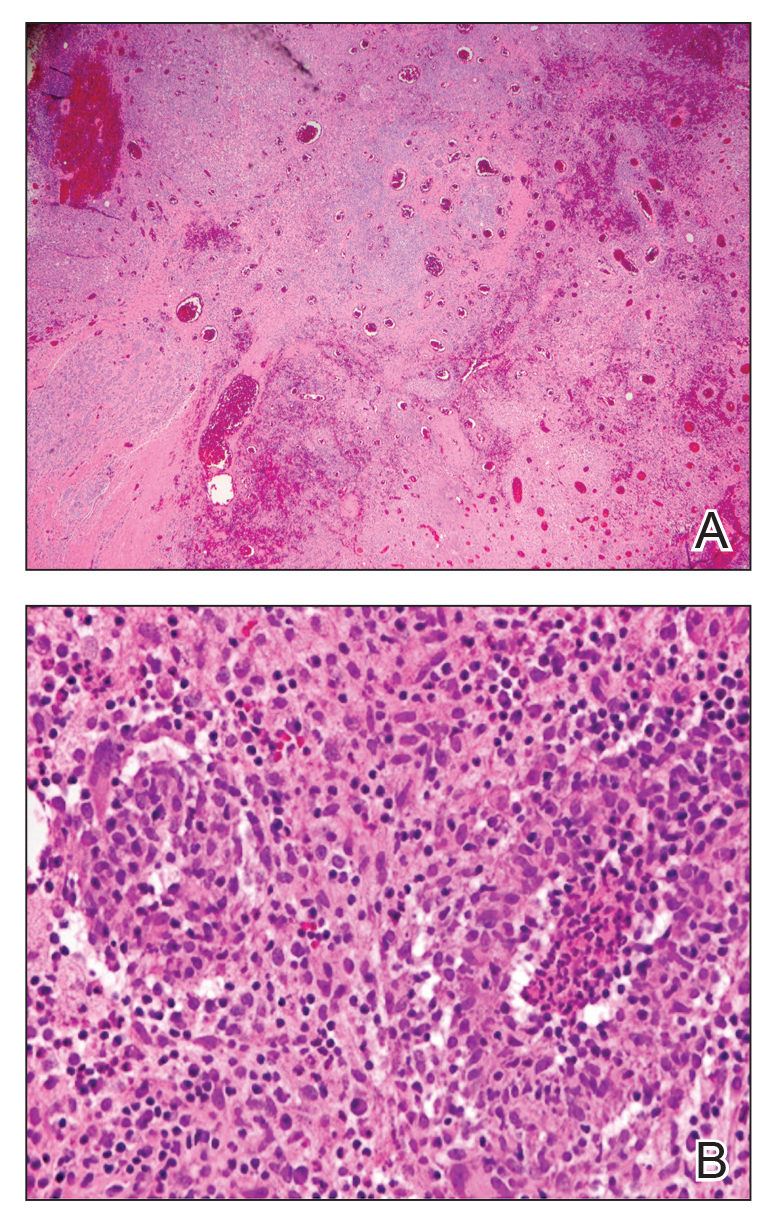
Breast biopsy showed tissue with large expanses of histiocytes, neutrophils, lymphocytes, plasma cells, and multinucleated giant cells (Figure 3A). Many discrete granulomas were seen against this mixed inflammatory background, associated with focal fat necrosis (Figure 3B). Special stains were negative for microorganisms. Histologic findings were consistent with granulomatous mastitis.
Referral to Dermatology
On presentation to dermatology, the patient was worked up for a possible granulomatous etiology, which included a negative PPD, as well as a normal chest radiograph, serum Ca2+ and ACE levels, and ophthalmology examination. Review of symptoms (ROS),medical history, and medication review were unremarkable.
By exclusion, the patient was given a diagnosis of IGM and started on methotrexate (15 mg weekly) with folic acid (1 mg daily). The condition of the right breast improved within 4 weeks of starting methotrexate; however, methotrexate was increased to 30 mg weekly because of occasional flares. The patient remained on methotrexate without further IGM flares for 8 months compared to prior unremitting pain and drainage. She was then tapered from methotrexate over 6 weeks without additional flares.






