Assessing benefits and risks of hormone therapy in 2008: New evidence, especially with regard to the heart
ABSTRACT
Observational studies, including the observational component of the Women's Health Initiative, consistently found that women who chose to use menopausal hormone therapy (HT) had a reduction in mortality and cardiovascular disease incidence relative to women who did not use HT. Randomized controlled trials have taught us that initiation of HT in older women (> 60 years old) remote from menopause (> 10 years since menopause) potentially has more risk than benefit. Additionally, randomized controlled trials have confirmed observational studies indicating the safety and benefit of HT in young (< 60 years old) recently menopausal women (< 10 years since menopause). In other words, we have come full circle in our understanding of HT, with a caveat concerning initiation in older women. Importantly, the magnitude and types of risk associated with HT are similar to those of other commonly used therapies. These data have led to recommendations that the benefits of HT exceed the risks when initiated in menopausal women younger than 60 years.
Physicians and their women patients have faced a continuous, confusing mix of information about the risks and benefits of hormone therapy (HT) for perimenopausal and postmenopausal women, most of it without respect to age or the timing of HT relative to menopause. Initial data from the Women’s Health Initiative (WHI) estrogen + progestin (E+P) trial, a prevention study conducted predominantly in older postmenopausal women without menopausal symptoms,1 resulted in questioning of the role of HT (unfortunately and inappropriately in younger symptomatic women). Cumulative trial data and further analyses of the WHI have refined and added to our understanding of the effects of HT, particularly with regard to cardiovascular health. This review will update physicians on the latest data on the risks and benefits of HT, with a particular focus on the heart, and will put the risks of HT into appropriate clinical context.
HORMONE THERAPY AND CARDIOVASCULAR DISEASE: A HISTORICAL PERSPECTIVE
Observational studies conducted prior to the WHI found consistently that women who self-selected to use HT had a reduction in mortality and in the incidence of cardiovascular disease relative to women who did not choose to use HT.2–8 This reduction in risk was apparent whether the HT users had taken ET (estrogen therapy) or EPT (estrogen-progestogen therapy). In contrast, randomized controlled trials failed to confirm these findings from observational studies. However, the findings from randomized controlled trials were derived from older postmenopausal women who were many years past menopause. Often overlooked is the WHI observational study of ET and EPT,9,10 in which women who chose to use HT had a reduction in the risk of coronary heart disease (CHD) similar to that observed among the HT users in other observational studies.
RECENT REPORTS FROM THE WHI
Since the original publication of the WHI E+P trial in 2002,1 an extensive collection of data have been published in piecemeal fashion, contributing to the confusion and misperception of the effects of HT on risks and benefits. It is important to note that the WHI consists of both randomized and observational components, as detailed below, and that data have come from both. Together, these data help clarify the misperceptions generated from the first WHI report of 2002,1 particularly misperceptions regarding the timing of HT initiation relative to menopause and the effect of HT duration on cardiovascular disease outcomes. In most instances, the conclusions drawn from this recent research run counter to the inaccurate but prevalent perception that HT use at any time and at any age is associated with cardiovascular harm, a perception that has unfortunately prevailed since the initial publication of the WHI E+P trial findings in 2002.
The WHI randomized trials and combined analysis
The WHI trials enrolled 27,347 postmenopausal women aged 50 to 79 years at baseline; almost two-thirds of the women enrolled were 60 years of age or older, and the majority of women were more than 10 years past menopause. WHI actually comprised two parallel randomized trials:
- One among 16,608 women who had not undergone hysterectomy (ie, with uterus intact), who were randomized to EPT or placebo (ie, WHI E+P trial) 1
- One among 10,739 women who had undergone hysterectomy, who were randomized to ET or placebo.11
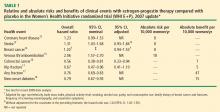
Recent analyses from the WHI, published in 2007, assessed the cardiovascular effects of ET and EPT independently and combined, both overall and according to subject age and years since menopause when randomized.12 Other analyses following the initial WHI E+P trial publication have analyzed the effects of HT according to duration of HT use and according to secondary end points. Many of these analyses have presented risks and benefits in terms of both nominal and adjusted confidence intervals (CIs). Nominal 95% CIs describe the variability in risk estimates that would arise from a simple trial for a single end point. Although nominal CIs are traditionally used, they do not take into account the multiple statistical testing issues (across time and across outcome categories) that occur in a trial. In contrast, adjusted 95% CIs correct for these stastical testing issues. From a clinical perspective, it is most appropriate to look at the adjusted CIs.
WHI: EPT vs placebo
CHD. Although the point estimate for CHD is increased, the 95% CI indicates that EPT has a non-significant effect on CHD outcome relative to placebo among all women randomized in the WHI E+P trial (mean age, 63 years).12 This is a very important point for cardiologists and primary care physicians to note.
In a 2008 analysis of the WHI E+P trial that included a 2.4-year open-label follow-up subsequent to the randomized trial,19 the randomized trial data reported were again different than in previous reports, but remained nonsignificant. The hazard ratio (HR) reported for CHD in the 2008 analysis for the randomized portion of the trial was 1.22 (95% CI, 0.99 to 1.51), as compared with 1.23 (95% CI, 0.99 to 1.53) reported in 200712 (Table 1), 1.24 (95% CI, 1.00 to 1.54) reported in 2003,20 and 1.29 (95% CI, 1.02 to 1.63) reported in 2002.1 In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens (EPT or placebo), the HR for CHD between the original randomized treatment groups was nonsignificant at 0.95 (95% CI, 0.73 to 1.26) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Stroke. The risk of stroke was increased significantly (by an additional 8 events per 10,000 women treated per year) in the EPT arm versus the placebo arm in the nominal analysis,12 but this difference was nonsignificant after adjustment.13
In the 2008 WHI E+P analysis, the HR reported for stroke during the randomized trial phase was different than in previous reports—1.34 (95% CI, 1.05 to 1.71)19 versus 1.31 (95% CI, 1.03 to 1.68) reported in 200712 (Table 1)—and the adjusted analysis was not reported. In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens, the HR for stroke between the original randomized treatment groups was nonsignifi-cant at 1.16 (95% CI, 0.83 to 1.61) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Breast cancer. Breast cancer risk was originally reported to be increased significantly (by an additional 8 cases per 10,000 women per year) in the EPT arm versus the placebo arm with the nominal statistic, but this increase was nonsignificant after adjustment.1 This risk estimate was revised in a follow-up publication 1 year after the original data were reported, and the increase in risk in the EPT arm was still no longer significant in the adjusted analysis.21 Importantly, another subsequent analysis that adjusted for baseline risk factors for breast cancer resulted in a further revision of the risk estimate, which again showed a nonsignificant increase in the EPT arm relative to the placebo arm.14 This is very important since it is commonly accepted that EPT increases the risk of breast cancer when this has not been definitively proven in any randomized controlled trial.
Unfortunately, the most recent breast cancer data14 (Table 1) were not used in the 2008 WHI E+P analysis.19 However, even using the unadjusted data in the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR for breast cancer between the original randomized treatment groups was nonsignificant and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Venous thromboembolism (VTE). EPT was associated with a doubling of the risk of VTE (ie, deep vein thrombosis and pulmonary embolism) compared with placebo, resulting in an excess of 18 VTE events per 10,000 women per year of therapy.15 The risk of VTE was significant across the entire cohort of women (mean age, 63 years).
In the 2008 WHI E+P analysis, the HR reported for VTE during the randomized phase was different than in previous reports—1.98 (95% CI, 1.52 to 2.59)19 versus 2.06 (95% CI, 1.57 to 2.70) reported in 200415 (Table 1)—and the HR during the 2.4-year open-label follow-up, in which women were no longer on their randomized regimens, was no longer significant (HR = 0.95; 95% CI, 0.63 to 1.44). This change in the HR over time from the randomized phase to the open-label phase was statistically significant.19
Fracture. The risk of hip fracture was reduced by 33% with EPT relative to placebo, which was statistically significant in the nominal analysis but not in the adjusted analysis.17 The risk of any fracture was reduced by 24% in women randomized to EPT compared with placebo, which was statistically significant and translated to 47 fewer fractures per 10,000 women per year of therapy.17 Clinically, these results are most impressive given that women randomized in the WHI were not selected on the basis of risk for osteoporosis or fracture. This claim cannot be made for any other therapy.
In the 2008 WHI E+P analysis of the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR between the original randomized treatment groups was nonsignificant for hip fracture and any fracture—0.92 (95% CI, 0.64 to 1.34) and 0.91 (95% CI, 0.78 to 1.06), respectively—and the change in the HR over time from the randomized phase to the open-label phase was not significant for either fracture outcome.19
Diabetes. The risk of new-onset diabetes was reduced by a statistically significant 21% in women randomized to EPT compared with placebo.18