Evaluating brain function in patients with disorders of consciousness
ABSTRACT
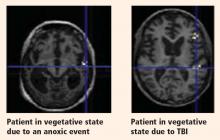
Evaluating brain function in patients with disorders of consciousness may offer important clues to their state of awareness and help to predict prognosis. Disorders of consciousness mainly comprise the comatose state, the vegetative state, and the minimally conscious state. These disorders typically stem from acute brain insults caused by hypoxic-ischemic neural injury or traumatic brain injury, and the type of brain injury frequently determines the neuropathology. Current knowledge, including results from our laboratory, supports a model of extended brain tissue damage from the midbrain to the cortex in anoxia patients and a model of focal or multifocal cortical lesions in trauma patients. These differing models may help to explain differences in prognosis and outcomes in these excruciating life situations. Although the neural basis of consciousness remains puzzling, findings from normal volunteers and pathologies of consciousness show that widely distributed networks such as thalamofrontal and parietofrontal systems may be critical.
DETERMINING AWARENESS WITHOUT REPORT
The proposed neural correlates of consciousness do not usually take into account the levels of consciousness.15,16 In order to build the framework for a cognitive neuroscience of consciousness, we must consider the content of the consciousness experience in fully awake subjects and patients as well as the cognitive processes occurring in unconscious and conscious subjects.
Two main approaches can be used to assess conscious processing in unresponsive patients. The first is to look for neural correlates in direct intentional actions or imagined actions,11 and the second is to look for physiologic correlates of the cognitive processes required during the conscious processing of stimuli.17
Searching for neural correlates of intended actions
The first approach can have enormous impact in the diagnostic arena (as well as in the legal and ethical arenas), such as in the case reported by Owen et al in which a patient showed brain activity related to imagining actions as prompted by spoken instructions during fMRI evaluation.11 Unfortunately, cases such as these are scarce. Moreover, imagining of actions relies not only on a spared comprehension capacity and preserved memory but also on the subject’s willingness to perform the task. It would seem that only a minority of patients in a vegetative state seem to have the cognitive abilities preserved to accomplish these types of tasks.
Searching for physiologic correlates of cognitive processes
The second approach would tend to work with memory and switching attention capabilities in unresponsive patients, assuming that conscious processing does not exist without these cognitive processes. The evidence for this approach comes from electrophysiology. Cognitive evoked potentials are commonly applied to assess basic auditory or visual cortical processing, automatic attention, and focus attention.18 Both the mismatch negativity wave (a correlate of automatic attention) and the p300 (a correlate of focus attention) are sometimes present,19 specifically in patients in vegetative or minimally conscious states, and they are a good predictor of awakening in stroke, hemorrhage, and traumatic brain injury.20
In day-to-day practice in a neurology clinic or emergency room, it is more feasible to assess cognitive capabilities using event-related potentials than fMRI since they are more widely distributed, more easily validated, shorter, and statistically more powerful in single-subject analysis,21 and because they do not frequently rely on speech comprehension.
NEUROPATHOLOGY AND fMRI
The cause of the brain injury leading to a vegetative or minimally conscious state frequently determines the neuropathology.22 It has also been demonstrated that severely disabled patients (such as those emerging from a minimally conscious state) differ from vegetative state patients in terms of lesions and severity.23
Although residual activity as seen on functional neuroimaging may be unequivocal in some cases, it may represent only fragmentary cognitive processing; it is important not to assume that normal awareness is present. Much still needs to be learned, but results from neuroimaging studies demonstrate that a small proportion of patients in a vegetative or minimally conscious state have some preserved cognitive processes. These findings have ethical and legal implications. For instance, careless bedside chatter among family members or medical personnel is inappropriate and should be avoided. Whether functional neuroimaging can effectively evaluate neuroprocessing in patients in whom cognitive output is difficult to assess remains to be determined. Such evaluation may one day help to predict prognosis. It may also someday help to facilitate communication with patients with locked-in syndrome, who are cognitively intact but are without verbal or motor output.
CONCLUSIONS
It is highly improbable to find patients with preserved cortical connectivity, since structural22 and functional19 studies have demonstrated only a small proportion of patients in a vegetative or minimally conscious state who have relatively preserved brains and cognitive processing. The more we study patients who are unresponsive or show low levels of response, the more complex cognitive processes we find in subpopulations of these patients. Language-related cortical activation is now the most common finding.13,19,24 More recently, a few researchers working with severely damaged patients have started to test paradigms with the aim of uncovering conscious processes that have no need of verbal or movement responses.
The time has come for clinicians in acute care centers to immediately follow their administration of coma scales in unresponsive patients with the use of more sophisticated methodology to assess not only reflexive and intentional behaviors but also these patients’ physiologic and cognitive characteristics. In the field of neurodegenerative disease, it took several years for clinicians to start using more sensitive cognitive tools than just the mini-mental state examination and computed tomography or three-dimensional T1-weighted structural MRI, but nowadays volumetric MRI and detailed cognitive assessments are widely used to diagnose and characterize patients with neurodegenerative disorders. The same path should be taken for patients with severe brain damage. The information yielded by such an approach may one day help to determine a diagnosis or prognosis, guide treatment, or facilitate communication in patients with pathologies of consciousness.