Evaluating brain function in patients with disorders of consciousness
ABSTRACT
Evaluating brain function in patients with disorders of consciousness may offer important clues to their state of awareness and help to predict prognosis. Disorders of consciousness mainly comprise the comatose state, the vegetative state, and the minimally conscious state. These disorders typically stem from acute brain insults caused by hypoxic-ischemic neural injury or traumatic brain injury, and the type of brain injury frequently determines the neuropathology. Current knowledge, including results from our laboratory, supports a model of extended brain tissue damage from the midbrain to the cortex in anoxia patients and a model of focal or multifocal cortical lesions in trauma patients. These differing models may help to explain differences in prognosis and outcomes in these excruciating life situations. Although the neural basis of consciousness remains puzzling, findings from normal volunteers and pathologies of consciousness show that widely distributed networks such as thalamofrontal and parietofrontal systems may be critical.
DEFINITION PROBLEMS AND MISDIAGNOSIS
The diagnosis of vegetative state emerges from a negative finding—namely, the lack of behaviors that would signal conscious capabilities. Using the nonoccurrence of events as a criterion to establish a fact is inherently problematic, since the causes of a nonoccurrence are theoretically infinite. More specifically, the reasons behind the lack of evidence of voluntary movement in presumably unconscious patients can be classified in terms of malfunctioning of either sensoriperceptual, output/motor, or central processing.
Deficits in sensoriperceptual processing
A patient might have deafness that may lead to a deficit in speech comprehension, or perhaps the auditory pathway and first cortical pathways are spared but the patient is aphasic and cannot process additive events such as speech. In a cohort of 42 patients, we found 17 who lacked the fourth or fifth components of the brain auditory evoked potentials to clicks presented binaurally, signaling severe damage to the auditory pathway.8 It is useless to ask such patients to follow commands, since the sensory input is damaged and the movement (or lack of movement) has no validity for the diagnosis. A similar argument can apply for patients who may show some fixation but exhibit delayed or absent visual evoked potentials when presented with written commands.
Deficits in motor processing
The second type of lesions that may contribute to misdiagnosis in these patients are those found in the effector systems. If the motor voluntary pathways are damaged—either in the motor cortex or in the corticospinal or corticobulbar pathways—then movement might be impaired enough to prevent responses by the patient. Patients of this type are sometimes diagnosed as being in a vegetative state although they might actually have locked-in syndrome,9 with preserved cognition but an inability to initiate voluntary responses as a result of a lesion in the pontine peduncle.
Although the effector systems are difficult to test in unresponsive subjects, some strategies may be tried. Before testing for volition, it is necessary to assess all possible hand, leg, and face reflexes in order to map reflexive behavior. Commands should then specifically target those muscles that showed total or partial preservation of reflexes. To test the output pathways from the cortex to the medulla, a more specialized assessment is needed; the Impaired Consciousness Research Group at the University of Cambridge has developed a simple protocol to assess the ability of the motor cortex to elicit muscle twitches by measuring the motor evoked potentials to simple pulses of transcranial magnetic stimulation. The minimal pulse intensity is determined by electromyographic recordings when transcranial magnetic stimulation pulses are applied to the left or right motor cortices for the hands and feet. The results have shown 2 out of 34 patients to have no detectable motor evoked potentials and 5 patients to have severe delay at maximum pulse intensity [unpublished data]. These results confirm the need for a full neurologic and neurophysiologic assessment in subjects who are unresponsive or show low levels of response, both acutely and more chronically, to minimize the risk of misdiagnosis.
Deficits in central processing
The key element in the assessment of cognitive processing in patients in a vegetative or minimally conscious state is determining deficits in their capacity to process external stimuli in a conscious manner (central processing). This is by far the most difficult characteristic to be determined since the only accepted criteria for awareness are verbal report or voluntary movement, both of which are absent in the vegetative state and are inconsistent and difficult to determine behaviorally in the minimally conscious state.
CLUES TO BRAIN FUNCTION IN DISORDERS OF CONSCIOUSNESS
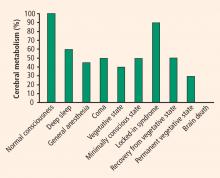
It is important to differentiate a patient in a persistent vegetative state from a patient in a minimally conscious state, as the latter patient has a much higher chance of a favorable outcome. Evaluation of cerebral metabolism and imaging studies can both provide clues to brain function.
Cerebral metabolism
Neuroimaging studies
In the past few years, studies have found that some patients in a vegetative or minimally conscious state can activate cortical networks in response to auditory, visual, and tactile stimuli.10 A challenge in neuroscience is to devise a reliable, objective test to assess awareness without relying on explicit voluntary movements or verbal responses. Such a test would have important theoretical and practical implications. Recent evidence from functional neuroimaging and neurophysiology suggests that some patients with disorders of consciousness exhibit partially preserved conscious processing despite having no clinical or verbal output.11
During a positron emission tomography study, Menon et al showed photographs to a 26-year-old woman who was in a vegetative state 4 months after becoming comatose from an acute febrile illness.12 They found significant activation in the right fusiform gyrus and extrastriate visual association areas when the woman was shown photos of people familiar to her as compared with repixellated versions of the same photos with the faces made unrecognizable. The activation pattern she exhibited was similar to that of healthy volunteers. Interestingly, a few months after this study, the patient became increasingly responsive.
Our group conducted the first evaluation of emotion in the minimally conscious state using functional MRI (fMRI) in a 17-year-old male following a traumatic brain injury.13 The patient was able to localize noxious stimuli, exhibited spontaneous eye opening, and occasionally smiled appropriately and followed people with his eyes. Imaging was performed while he listened to two recordings—one of his mother reading a story about his life, and one of a matched control voice reading the same story. Digital subtraction imaging disclosed strong activation of two areas related to emotion, the amygdala and the bilateral insula, while the recording of the patient’s mother was played. Activation was also evident in the auditory cortex in the superior temporal lobe. The patient recovered 6 months following this study.
Classical conditioning
Classical conditioning represents an alternate approach to MRI for assessing brain function in patients with disordered consciousness.8 Trace conditioning of the eye-blink response is considered to be an objective test of awareness.14 This test involves highly specific learning, requiring an anticipatory electromyographic response to a paired stimulus (eg, a tone followed by an aversive stimulus such as an air puff to the eyes) but not to an unpaired stimulus (eg, a white noise that is not followed by an aversive stimulus). This effect increases in amplitude as the aversive stimulus approaches. Our laboratory is applying this method to study learning and memory in patients with disordered consciousness.