Evaluating brain function in patients with disorders of consciousness
ABSTRACT
Evaluating brain function in patients with disorders of consciousness may offer important clues to their state of awareness and help to predict prognosis. Disorders of consciousness mainly comprise the comatose state, the vegetative state, and the minimally conscious state. These disorders typically stem from acute brain insults caused by hypoxic-ischemic neural injury or traumatic brain injury, and the type of brain injury frequently determines the neuropathology. Current knowledge, including results from our laboratory, supports a model of extended brain tissue damage from the midbrain to the cortex in anoxia patients and a model of focal or multifocal cortical lesions in trauma patients. These differing models may help to explain differences in prognosis and outcomes in these excruciating life situations. Although the neural basis of consciousness remains puzzling, findings from normal volunteers and pathologies of consciousness show that widely distributed networks such as thalamofrontal and parietofrontal systems may be critical.
Consciousness has long been a fascinating subject to both philosophers and scientists, yet consciousness has only recently been taken into account by neuroscientists as a topic for research. This article discusses research done over the past 10 years evaluating brain function in patients with disorders of consciousness—specifically those in a vegetative or minimally conscious state. We highlight physiologic, sensory, perceptual, cognitive, and behavioral commonalities and disparities between patients with anoxic and traumatic brain injuries, with the aim of characterizing the neurophysiologic and neuroanatomic differences between these two main causes of disorders of consciousness.
WHAT IS CONSCIOUSNESS?
Although consciousness is difficult to describe, it can be defined as a combination of wakefulness and awareness.1 As for the brain systems supporting these two aspects of consciousness, it has been suggested that the brainstem ascending reticular formation system and its thalamic projections support alertness and the sleep-wake cycle, and that conscious awareness relies on a functional thalamocortical and corticocortical system.
DISORDERS OF CONSCIOUSNESS: A VARIETY OF STATES
Coma: Near-complete unresponsiveness
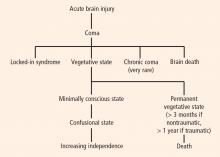
Coma is a condition of almost complete unresponsiveness in which the patient lies with eyes closed, very limited reflexes, no cyclical wakefulness, and, above all, no signs of awareness. Coma is normally attained after an acute brain insult and may last about 2 weeks, although chronic coma cases have been described, and is usually caused by either temporary or permanent damage to the reticular system.
Vegetative state: Wakefulness without awareness
Following a coma, some patients may enter a vegetative state, which involves a complete absence of consciousness of one’s environment but with preserved sleep-wake cycles and autonomic functions. The vegetative state is easily differentiated from brain death, in which the electroencephalogram shows no brain wave or activity.4 Brain death is the irreversible end of all brain activity and should not be confused with a persistent vegetative state.
The vegetative state is a condition of wakefulness without awareness in which the patient exhibits a partially preserved sleep-wake cycle and a variable portfolio of reflexes and spontaneous nonvolitional behaviors. A patient who has been in a vegetative state for more than 1 month with no improvement is often said to be in a persistent vegetative state. The term permanent vegetative state, implying no chance of recovery, is sometimes used when the vegetative state persists for 3 months after a nontraumatic insult, such as cardiac arrest, or for 1 year after a traumatic brain injury.
Minimally conscious state: Conscious awareness is evident despite impairment
Some patients in a vegetative state may start to recover by entering a minimally conscious state, in which conscious awareness is evident despite profound physical and cognitive impairment. Although communication capabilities are absent, cognitively mediated (or voluntary) behavior occurs in the minimally conscious state, which may be inconsistent but is reproducible enough to be differentiated from reflexive behavior. For example, patients may occasionally be able to smile when asked to do so or follow an object with their eyes. In the minimally conscious state, patients show those basic behaviors seen in the vegetative state along with islands of presumably conscious processing such as inconsistent responses to simple commands and sustained visual pursuit.5 Patients in a minimally conscious state have a better prognosis than those in a persistent or permanent vegetative state.3
Locked-in syndrome: Not a true disorder of consciousness
Another pathology that is often confounded with vegetative or minimally conscious states is the locked-in syndrome, which is characterized by complete paralysis of voluntary muscles in all parts of the body except those controlling eye movements. Individuals with locked-in syndrome are conscious and can think and reason, but they are unable to speak or move. The disorder confines the patient to paralysis and a mute state. Communication may be possible with blinking eye movements.
WHAT CAUSES DISORDERS OF CONSCIOUSNESS?
Disorders of consciousness mostly stem from acute brain insults, which may be caused by hypoxicischemic neural injury or traumatic brain injury. Although traumatic brain injury is currently the most common cause of vegetative and minimally conscious states, nontraumatic causes are becoming more frequent as a result of scientific and technological developments in resuscitation. Nontraumatic causes of disorders of consciousness include stroke, cardiopulmonary arrest, and meningoencephalitis; additionally, patients in the final stage of certain neurodegenerative diseases, including Parkinson, Alzheimer, and Huntington diseases, may lapse into a minimally conscious or vegetative state.6
NEUROLOGIC FINDINGS IN COMATOSE SURVIVORS OF CARDIAC ARREST
Structural magnetic resonance imaging (MRI) of patients in a vegetative state following cardiac arrest often reveals abnormalities. Most frequently there is a white matter signal in the cerebellum, the thalamus, the frontal and parietal cortices, and the hippocampus. Widespread abnormalities may indicate little to no prospect for recovery. Pupillary light response, corneal reflexes, motor responses to pain, myoclonus status epilepticus, serum neuron-specific enolase, and somatosensory evoked potential studies can assist in predicting efficiently and accurately a poor outcome in comatose patients after cardiopulmonary resuscitation for cardiac arrest.7