Sleep apnea and the heart
Release date: September 1, 2019
Expiration date: August 31, 2022
Estimated time of completion: 0.75 hour
Click here to start this CME activity.
ABSTRACT
The normal sleep-wake cycle is characterized by diurnal variations in blood pressure, heart rate, and cardiac events. Sleep apnea disrupts the normal sleep-heart interaction, and the pathophysiology varies for obstructive sleep apnea (OSA) and central sleep apnea (CSA). Associations exist between sleep-disordered breathing (which encompasses both OSA and CSA) and heart failure, atrial fibrillation, stroke, coronary artery disease, and cardiovascular mortality. Treatment options include positive airway pressure as well as adaptive servo-ventilation and phrenic nerve stimulation for CSA. Treatment improves blood pressure, quality of life, and sleepiness, the last particularly in those at risk for cardiovascular disease. Results from clinical trials are not definitive in terms of hard cardiovascular outcomes.
KEY POINTS
- Diurnal variations in blood pressure, heart rate, and cardiac events occur during normal sleep.
- While normal sleep may be cardioprotective, sleep apnea disrupts the normal sleep-heart interaction.
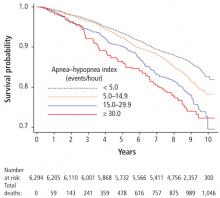
- Untreated severe sleep apnea increases the risk for cardiovascular events.
- Treatment with continuous positive airway pressure (CPAP) may reduce the risk of cardiac events based on some data, though randomized studies suggest no improvement in cardiovascular mortality.
- Poor patient adherence to CPAP makes it difficult to evaluate the efficacy of CPAP treatment in clinical trials.
SLEEP APNEA, CORONARY ARTERY DISEASE, AND CARIOVASCULAR MORTALITY
The association between sleep apnea and coronary artery disease and cardiovascular mortality was considered in a Spanish study of 1,500 patients followed for 10 years, which reported that CPAP therapy reduced cardiac events in patients with OSA.66 Patients with sleep apnea had an increased risk of fatal myocardial infarction or stroke. Survival of patients treated for sleep apnea approached that of patients without OSA.
In a study of a racially diverse cohort, an association of physician diagnosed sleep apnea with cardiovascular events and survival was identified.67 Diagnosed sleep apnea was estimated to confer a two- to threefold increase in various cardiovascular outcomes and all-cause mortality.
The effect of treatment for sleep apnea on cardiovascular outcomes was the focus of a recent randomized controlled trial of nearly 3,000 participants with a mean follow-up of 4 years.65 Use of CPAP compared with usual care found no difference in cardiovascular outcomes. However, secondary analysis revealed a possible benefit of a lower risk of stroke with use of CPAP therapy. Several factors should be considered in interpreting these findings: ie, low adherence with CPAP therapy (3 hours), whether the study was sufficiently powered to detect a change in cardiovascular outcomes, and if the duration of follow-up was adequate. In terms of patient demographics and study generalizability, the study did not include patients with severe sleep apnea and hypoxia, and most participants were men, of Asian descent, with a mean body mass index of 28 kg/m2, and low levels of sleepiness at baseline.