Decreasing Hypoglycemia following Insulin Administration for Inpatient Hyperkalemia
BACKGROUND: Acute hyperkalemia (serum potassium ≥ 5.1 mEq/L) is often treated with a bolus of IV insulin. This treatment may result in iatrogenic hypoglycemia (glucose < 70 mg/dl).
OBJECTIVES: The aims of this study were to accurately determine the frequency of iatrogenic hypoglycemia following insulin treatment for hyperkalemia, and to develop an electronic health record (EHR) orderset to decrease the risk for iatrogenic hypoglycemia.
DESIGN: This study was an observational, prospective study.
SETTING: The setting for this study was a university hospital.
PATIENTS: All nonobstetric adult inpatients in all acute and intensive care units were eligible.
INTERVENTION: Implementation of a hyperkalemia orderset (Orderset 1.1) with glucose checks before and then one, two, four, and six hours after regular intravenous insulin administration. Based on the results from Orderset 1.1, Orderset 1.2 was developed and introduced to include weight-based dosing of insulin options, alerts identifying patients at higher risk of hypoglycemia, and tools to guide decision-making based on the preinsulin blood glucose level.
MEASUREMENTS: Patient demographics, weight, diabetes history, potassium level, renal function, and glucose levels were recorded before, and then glucose levels were measured again at one, two, four, and six hours after insulin was administered.
RESULTS: The iatrogenic hypoglycemia rate identified with mandatory glucose checks in Orderset 1.1 was 21%; 92% of these occurred within three hours posttreatment. Risk factors for hypoglycemia included decreased renal function (serum creatinine >2.5 mg/dl), a high dose of insulin (>0.14 units/kg), and re-treatment with blood glucose < 140 mg/dl. After the introduction of Orderset 1.2, the rate of iatrogenic hypoglycemia decreased to 10%.
CONCLUSIONS: The use of an EHR orderset for treating hyperkalemia may reduce the risk of iatrogenic hypoglycemia in patients receiving insulin while still adequately lowering their potassium.
© 2020 Society of Hospital Medicine
Statistical Analysis
Statistical analysis for our data included the χ2 test for categorical data and Student t test for continuous data. The bivariate analysis identified potential risk factors and protective factors for hypoglycemia, and logistic regression was used to determine independent predictors of hypoglycemia. Through bivariate analyses, any factor with a P value below .05 was included in the multivariable analyses to investigate a significant contribution to hypoglycemia outcomes. Analyses for hypoglycemia and severe hypoglycemia rates, potassium levels pre- and postinsulin treatment, and hyperglycemia rates were done for both the intention-to-treat group and the group with all criteria met. All analyses were rendered utilizing Stata version 14 (Stata Corp LLC, College Station, Texas).
RESULTS
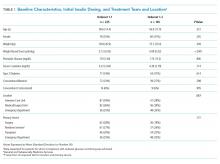
Baseline patient characteristics, initial insulin dosing, the treatment team, and the location are shown in Table 1. With the implementation of weight-based dosing, a lower dose of insulin was administered with Orderset 1.2 compared with Orderset 1.1.
Orderset adherence rates for Orderset 1.1 and 1.2 were as follows: Acute Care Floor 65% (70%), Intensive Care Unit 63% (66%), and Emergency Department 60% (55%). A two-month audit of orderset usage and compliance revealed that 73% (70 of 96) of insulin treatments were ordered through Orderset 1.1, and 77% (71 of 92) of insulin treatments were ordered through Orderset 1.2. The distribution of orderset usage across location and primary service are shown in Table 1.
The patient distribution is shown in the Figure. In the Orderset 1.1 period, there were 352 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 225 patients for whom compliance with orderset monitoring was achieved. Notably, 112 treatments were excluded for the lack of adequate blood glucose monitoring. In the Orderset 1.2 period, there were 239 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 145 patients for whom compliance with orderset monitoring was achieved. During this phase, 80 treatments were excluded for inadequate blood glucose monitoring.
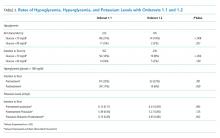
Predictors of hypoglycemia following the implementation of Orderset 1.1 are shown in Table 2, and the logistic regression model of these risks is shown in Appendix Table 1. Female gender, weight-based dosing of insulin exceeding 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dl were associated with an increased risk of hypoglycemia. A known diagnosis of Type 2 diabetes, concomitant albuterol within one hour of insulin administration, and corticosteroid administration within two hours of insulin administration were associated with a decreased risk of hypoglycemia.
The rates of hypoglycemia (<70 mg/dl) and severe hypoglycemia (<40 mg/dl) are shown in Table 3. During the Orderset 1.1 period,
During the Orderset 1.2 period, for patients with all criteria met, 14 of 145 (10%) had hypoglycemia, and three of 145 (2%) had severe hypoglycemia. Ten of 14 (72%) of these hypoglycemic events occurred in the first three hours, with the remaining four hypoglycemic events (28%) occurring in the last three hours.
An intention-to-treat analysis for hyperglycemia, defined as glucose >180 mg/dl, revealed that during the Orderset 1.1 period, 80 of 352 (23%) had hyperglycemia before insulin administration, and 38 of 352 (11%) had hyperglycemia after insulin administration. During the Orderset 1.2 period, 52 of 239 (22%) had hyperglycemia before insulin administration, and 15 of 239 (6%) had hyperglycemia after insulin administration. Results can be found in Table 3.
Pre- and posttreatment potassium levels are shown in Table 3. An intention-to-treat analysis for potassium reduction postinsulin administration revealed that during the Orderset 1.1 period, there was an absolute reduction of 0.73 mmol/L, while during the Orderset 1.2 period, there was an absolute reduction of 0.95 mmol/L.