Medical Comanagement of Hip Fracture Patients Is Not Associated with Superior Perioperative Outcomes: A Propensity Score-Matched Retrospective Cohort Analysis of the National Surgical Quality Improvement Project
BACKGROUND: Medical comanagement entails a significant commitment of clinical resources with the aim of improving perioperative outcomes for patients admitted with hip fractures. To our knowledge, no national analyses have demonstrated whether patients benefit from this practice.
METHODS: We performed a retrospective cohort analysis of the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) targeted user file for hip fracture 2016-2017. Medical comanagement is a dedicated variable in the NSQIP. Propensity score matching was performed to control for baseline differences associated with comanagement. Matched pairs binary logistic regression was then performed to determine the effect of comanagement on the following primary outcomes: mortality and a composite endpoint of major morbidity.
RESULTS: Unadjusted analyses demonstrated that patients receiving medical comanagement were older and sicker with a greater burden of comorbidities. Comanagement did not have a higher proportion of patients participating in a standardized hip fracture program (53.6% vs 53.7%; P > .05). Comanagement was associated with a higher unadjusted rate of mortality (6.9% vs 4.0%, odds ratio [OR] 1.79: 1.44-2.22; P < .0001) and morbidity (19.5% vs 9.6%, OR 2.28: 1.98-2.63; P < .0001). After propensity score matching was used to control for baseline differences associated with comanagement, patients in the comanagement cohort continued to demonstrate inferior mortality (OR 1.36: 1.02-1.81; P = .033) and morbidity (OR 1.82: 1.52-2.20; P < .0001).
CONCLUSIONS: This analysis does not provide evidence that dedicated medical comanagement of hip fracture patients is associated with superior perioperative outcomes. Further efforts may be needed to refine opportunities to modify the significant morbidity and mortality that persists in this population.
© 2019 Society of Hospital Medicine
RESULTS
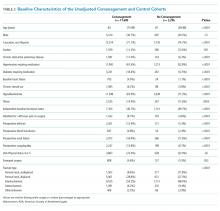
A total of 19,896 Hip fracture patients were categorized into a medical comanagement cohort of 17,600 (88.5%) patients and a cohort without comanagement of 2,296 patients (11.5%). Baseline characteristics of the two unadjusted cohorts before propensity score matching are presented in Table 2.
Patients in the comanagement cohort were older and sicker in terms of almost every comorbidity and condition evaluated (Table 2). These differences were also reflected in a higher predicted mortality by the NSQIP hierarchical regression-based equations for mortality (3.5% [1.7%-7.0%] vs 2.5% [0.9%-6.1%], P < .0001) and morbidity (9.1% [6.9%-12.5%] vs 8.5% [6.1%-12.1%], P ≤ .0001). As predicted, the observed, unadjusted rate of death in the comanagement cohort was higher than that in the cohort without comanagement: n = 1,210 (6.9%) vs n = 91 (4.0%), odds ratio (OR) 1.79: 1.44-2.22; P < .0001, as was the unadjusted rate of the composite endpoint of major morbidity: n = 3,425 (19.5%) vs n = 220 (9.6%), OR 2.28: 1.98-2.63, P < .0001. There was no difference in the prevalence of using an SHFP in the comanagement and noncomanagement cohorts (n = 9,441, 53.6% vs n = 1,232, 53.7%, P > .05).
Logistic regression modeling of the probability of membership in the comanagement cohort yielded satisfactory results (convergent model, null hypothesis rejected, area under the curve of the model receiver operating curve [AUROC] = 0.81). Propensity scores were calculated using the significant variables from this model, as detailed in Table 1. Propensity score matching was then performed with excellent results as follows: n = 2,278 of 2,296 (99.2%) potential pairs were successfully matched, residual absolute standardized difference = 0.0039 (99.7% reduction), variance ratio = 1.01. This satisfies the traditional criterion for a satisfactory variable balance in propensity score matching of a standardized difference ≤0.25 and a variance ratio between 0.5 and 2.0. It is also worthy of note that the propensity score matching process successfully eliminated the baseline difference in the NSQIP-predicted probability of mortality (2.7% [1.1%-5.8%] vs 2.5% [0.9%-6.2%], P = .15) and morbidity (8.6% [6.5%-11.7%] vs 8.6% [6.1%-12.2%], P = .80).
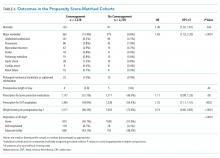
The characteristics of the propensity score-matched cohorts (n = 2,278 each) are shown in Table 3. Matching resulted in a satisfactory balance of measurable covariates between the two cohorts, with the exception of small (but statistically significant) differences in the prevalence of hypoalbuminemia and the distribution of fracture type.
The comanagement cohort did not experience superior results for either of the two primary outcomes mortality (OR 1.36: 1.02-1.81; P = .033) or in the composite endpoint of morbidity (OR 1.82: 1.52-2.20; P < .0001). The secondary outcomes of the two cohorts of patients are shown in Table 4. The comanagement cohort did not have superior outcomes in any variable examined, except for a slightly higher proportion of patients who were appropriately prescribed DVT prophylaxis. Despite the prophylaxis, the comanagement cohort did not have a smaller proportion of patients who experienced a DVT or PE.
Post hoc subgroup analysis was performed to assess whether comanagement demonstrated an association with improved outcomes depending on whether patients were or were not treated in an SHFP. This stratified analysis produced the same results as the primary analysis; ie, comanagement was not associated with improved outcomes in either subgroup.